Video: Predicting pathological outcomes in patients undergoing RARP for high-risk prostate cancer: A Preoperative Nomogram
Predicting Pathologic Outcomes in Patients Undergoing Robot-Assisted Radical Prostatectomy for High Risk Prostate Cancer: A Preoperative Nomogram
OBJECTIVE
To identify which high-risk patients with prostate cancer may harbour favourable pathological outcomes at radical prostatectomy (RP).
PATIENTS AND METHODS
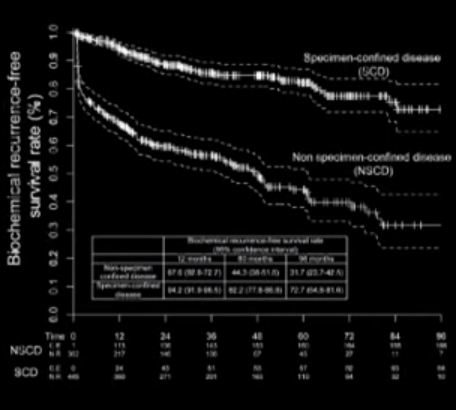
We evaluated 810 patients with high-risk prostate cancer, defined as having one or more of the following: PSA level of >20 ng/mL, Gleason score ≥8, clinical stage ≥T2c. Patients underwent robot-assisted RP (RARP) with pelvic lymph node dissection, between 2003 and 2012, in one centre. Only 1.6% (13/810) of patients received any adjuvant treatment. Favourable pathological outcome was defined as specimen-confined disease (SCD; pT2–T3a, node negative, and negative surgical margins) at RARP-specimen. Logistic regression models were used to test the relationship among all available predicators and harbouring SCD. A logistic regression coefficient-based nomogram was constructed and internally validated using 200 bootstrap resamples. Kaplan–Meier method estimated biochemical recurrence (BCR)-free and cancer-specific mortality (CSM)-free survival rates, after stratification according to pathological disease status.
RESULTS
Overall, 55.2% patients harboured SCD at RARP. At multivariable analysis, PSA level, clinical stage, primary/secondary Gleason scores, and maximum percentage tumour quartiles were all independent predictors of SCD (all P < 0.04). A nomogram based on these variables showed 76% discrimination accuracy in predicting SCD, and very favourable calibration characteristics. Patients with SCD had significantly higher 8-year BCR- (72.7% vs 31.7%, P < 0.001) and CSM-free survival rates (100% vs 86.9%, P < 0.001) than patients with non-SCD.
CONCLUSIONS
We developed a novel nomogram predicting SCD at RARP. Patients with SCD achieved favourable long-term BCR- and CSM-free survival rates after RARP. The nomogram may be used to support clinical decision-making, and aid in selection of patients with high-risk prostate cancer most likely to benefit from RARP.