Editorial: Analysis of Genetics to Identify Susceptibility to Secondary Malignancies in Patients with BCa
A study by Muller et al. [1] evaluated a cohort of 10 047 patients diagnosed with a first invasive (≥T1) bladder cancer and found that independent of gender and age, the risk of subsequent lung cancer was increased. This is not surprising considering the strong association of both bladder and lung cancer with tobacco, which is the main risk factor for both malignancies. While the authors limited their analysis to patients with invasive disease, the same association of bladder and lung cancer probably holds true for patients with non-invasive disease. An important question this raises is whether urologists should be more proactive in screening for lung cancer in their patients with bladder cancer. While chest radiographs are commonly used to monitor patients who undergo cystectomy, they are not routinely used for patients with non-invasive disease. Furthermore, the recommendations for screening for lung cancer based on the National Lung Cancer Screening Trial (NLST) involve use of low-dose chest CT, which is rarely done routinely by urologists [2]. In the Muller et al. [1] study, despite the large cohort and median follow-up of 3.1 years, there were still only 295 cases of lung cancer. This was three-times the expected incidence but overall a low rate.
One interesting consideration is whether use of genetic factors may be useful to identify which patients might be at higher risk at baseline for subsequent secondary cancers. Currently, single nucleotide polymorphism (SNP) analysis is not used clinically in screening but other genetic abnormalities such as BRCA (BReast Cancer gene) mutations and Lynch syndrome have been used to identify secondary malignancies. However, identifying individuals at higher risk of developing cancer may inform clinicians and allow for a more targeted screening strategy, even in patients of increased baseline risk.
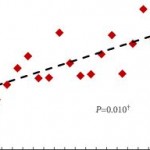
The USA National Cancer Institute performed genome-wide association studies (GWAS) for 49 492 patients with cancer and 34 131 controls to estimate the heritability of individual cancers, as well as the proportion of heritability attributable to cigarette smoking in smoking-related cancers, and the genetic correlation between pairs of cancers [3]. They calculated that at least 24% and 7% of the heritability for lung and bladder cancer, respectively, can be attributed to genetic determinants of smoking. Only four pairs of cancers had marginally statistically significant correlations including bladder and lung.
While tobacco is the major cause of lung cancer, only ≈10% of smokers develop lung cancer in their lifetime indicating there is significant individual variation in susceptibility to lung cancer. The International Lung Cancer Consortium pooled genotype data for SNPs at chromosomes 15q25 (rs16969968, rs8034191), 5p15 (rs2736100, rs402710), and 6p21 (rs2256543, rs4324798) from 21 case-control studies for 11 645 patients with lung cancer and 14 954 control subjects [4]. Associations between 15q25 and the risk of lung cancer were replicated in White ever-smokers (rs16969968) but there was no association in never-smokers or in Asians between either of the 15q25 variants and the risk of lung cancer. For the chromosome 5p15 region, they confirmed statistically significant associations in Whites for both rs2736100 and rs402710 and identified similar associations in Asians. Zhang et al. [5] undertook a gene–smoking interaction analysis in a GWAS of lung cancer in Han Chinese population of 5 408 subjects (2 331 patients and 3 077 controls) using a two-phase designed case-control study. They identified two SNPs associated with lung cancer and smoking, including one with a synergistic interaction (rs4589502) and one with an antagonistic interaction (rs131629).
There have also been several studies evaluating SNPs and risk of bladder cancer. A study of 1 595 patients and 1 760 controls, stratified for smoking habits, found that different SNP combinations were relevant in smokers and non-smokers [6]. In smokers, polymorphisms involved in detoxification of cigarette smoke carcinogens were most relevant (GSTM1 [glutathione S-transferase μ1], rs11892031), in contrast to those in non-smokers where MYC (v-myc avian myelocytomatosis viral oncogene homolog) and APOBEC3A (apolipoprotein B mRNA editing enzyme, catalytic polypeptide-like 3A) near polymorphisms (rs9642880, rs1014971) were the most influential. A study of genome-wide interaction of smoking and bladder cancer risk based on data from 3 002 patients and 4 411 controls with validation in a separate dataset identified 10 SNPs that showed association in a consistent manner with the initial dataset and in the combined dataset, providing evidence of interaction with tobacco use [7]. These studies of genetic polymorphisms add evidence regarding the impact of gene–environment interactions, which influence the detrimental effects of tobacco on risk of bladder cancer.
There are other genetic polymorphisms that have been found to increase risk of tobacco-related malignancies. A study of polymorphisms inNAT2 (N-acetyltransferase 2 [arylamine N-acetyltransferase]), GSTM1, NAT1, GSTT1 (GST θ1), GSTM3, and GSTP1 (GST π1) in 1 150 patients with bladder cancer and 1 149 controls found that compared with NAT2 rapid or intermediate acetylators, NAT2 slow acetylators had an increased overall risk of bladder cancer (odds ratio 1.4, 95% CI 1.2–1.7), which was stronger for cigarette smokers than for never smokers. No significant associations were found with the other polymorphisms [8]. The overall association for GSTM1 was also robust (P < 0.001) but was not modified by smoking status (P = 0.86).
While it may be too early to apply GWAS to all patients who smoke, a trial focusing on those with other tobacco-related malignancies may identify cohorts where screening for other malignancies is not only effective but also practical.