Editorial: Bringing clarity or confusion? The role of prostate-specific membrane antigen positron-emission/computed tomography for primary staging in prostate cancer
The use of 68Ga-labelled prostate-specific membrane antigen (PSMA) positron-emission tomography (PET)/CT for staging prostate cancer in Australia has reached almost plague-like proportions. Despite what must be admitted is little high-level evidence to guide us in the accuracy or appropriateness of this imaging technique for either primary staging or prostate cancer recurrence, hundreds of these scans are being performed every week around Australia, and in many cases we simply do not know what to do with the results. We performed the first such scan at our centre in Melbourne in August 2014, and were soon receiving 10 requests per day, with patients waiting up to 3 months to be scanned. Fast-forward 2 years, and there are now eight centres offering PSMA PET/CT in Melbourne, a city of 4.5 million people. Scans can be obtained within 24 h of referral and costs have dropped to €500. A similar situation exists in Germany where this imaging method was pioneered [1], and interest is also growing in Belgium, Italy, India and a number of other countries (the USA being a notable exception). But do we really understand the impact of the decision to perform PSMA/PET scanning, and do we have enough evidence to guide us on the most appropriate setting for its use?
The current interest in PSMA PET/CT has been triggered by the development of small molecule ligands which bind to the extracellular domain of the PSMA molecule, leading to increased sensitivity and specificity when compared with conventional imaging [2]. Previously, the use of PET imaging for prostate cancer detection was greatly limited by the relatively poor performance characteristics of choline-based PET/CT, and limited availability and high costs associated with this type of imaging. The introduction of 68Ga-labelled PSMA PET/CT has addressed many of these concerns, although high-quality evidence is still lacking to help guide its most appropriate utility. The best data exist for identification of prostate recurrence in patients with biochemical recurrence (BCR) after previous definitive therapy. In our recent systematic review and meta-analysis of this topic, we reported pooled data on 1309 men with BCR undergoing PSMA PET/CT [3]. When stratified by PSA level post-radical prostatectomy, positive scans are reported in 42, 58, 76 and 95% of patients with PSA levels of 0–0.2, 0.2–1, 1–2, and >2 ng/mL, respectively. Fewer data exist for the role of PSMA PET/CT in the primary staging setting.
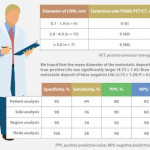
In this interesting paper from some of our Australian colleagues, van Leeuwen et al. [4] report their experience of PSMA PET/CT in the primary staging setting, in particular to evaluate the performance of PSMA PET/CT to evaluate lymph node positivity in patients with intermediate- and high-risk disease, scheduled for radical prostatectomy. A total of 30 patients underwent preoperative PSMA PET/CT, of which 27 were stratified as high risk, and all subsequently underwent radical prostatectomy and pelvic lymph node dissection. In total, 11 patients (37%) had histologically proven lymph node metastases. On a per-patient basis, PSMA PET had a sensitivity of 64%, specificity of 95%, positive predictive value of 88%, and negative predictive value of 82%. The average size of positive lymph nodes not detected by PSMA PET/CT was 2.7 mm; therefore, in this population of patients with predominately high-risk prostate cancer, PSMA PET/CT had very high specificity and moderate sensitivity for lymph node metastasis detection.
In a larger experience from Munich, Maurer et al. [5] compared pathology findings of 130 patients with intermediate- and high-risk disease who underwent radical prostatectomy and pelvic lymph node dissection, with preoperative PSMA PET/CT or PET/MRI findings. They reported similar sensitivity, specificity and accuracy of 65.9, 98.9 and 88.5%, respectively. On receiver-operating characteristic analysis, PSMA-PET performed significantly better than conventional imaging alone on patient and template-based analyses (P = 0.002 and <0.001, respectively).
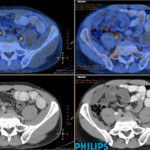
Just as there appears to be some clarity, however, in the role of PSMA PET/CT in patients with BCR, and in improving the detection of lymph node metastases preoperatively, there are many instances in which the high specificity of this scanning method leaves us in a decision-making quandary. As van Leeuwen et al. identified in their paper, and as we have frequently observed ourselves, PSMA PET/CT may identify prostate cancer in hitherto unidentified and unusual locations such as the mesorectum (Fig. 1). Disease may also be identified in quite distant locations despite relatively low PSA levels, thereby disrupting traditional management algorithms including the use of postoperative radiotherapy [6]. Should we alter patients’ management based on novel imaging, or should we assess the decision impact more formally in prospective studies? The answer should obviously be the latter, but the current plague of PSMA PET imaging means such decisions are already being taken in the absence of high-quality evidence.
Figure 1. 68Ga-labelled prostate-specific membrane antigen (PSMA) positron-emission tomography (PET)/CT in a 72-year-old man with biochemical recurrence after previous radical prostatectomy. His PSA level was 0.21 ng/mL and conventional staging including CT and bone scan showed no evidence of disease. PSMA PET/CT demonstrates intense avidity in an 11-mm mesorectal node near the recto-sigmoid junction on the left side. (a) CT demonstrates non-specific findings in area of subsequent avidity; (b) PSMA PET raw data demonstrating avidity in mesorectal node; (c) fused PSMA PET/CT image provides anatomical correlation; (d) coronal fused PET/CT image.
Nonetheless, PSMA PET imaging is here to stay, and will doubtless have a positive impact in improving decision-making in prostate cancer management as a result of the more accurate staging which it heralds. We must await more formal evaluation of the decision impact before defining the patient population who will benefit the most from this exciting imaging method.