Editorial: To drain or not to drain after RARP? That is the question
In the current issue of BJUI, the article by Chenam et al. [1] from the City of Hope Hospital clarifies an important surgical issue that most major uro-oncology centres face every day, but it also raises several other important surgical issues. The objective of the study was to determine if eliminating the routine placement of a pelvic drain after robot-assisted radical prostatectomy (RARP) affects the incidence of early (90-day) postoperative adverse events. RARP has become the new ‘gold standard’ approach for the surgical treatment of localized prostate cancer, and now comprises the majority of radical prostatectomies performed in the USA and the UK, with >80% of cases using this technique [2].
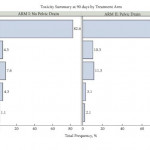
In this parallel-group, blinded, non-inferiority trial, patients who were planned to undergo RARP were randomized to one of two arms: no drain placement or pelvic drain placement. The primary endpoint was incidence of 90-day complications which, based on standard treatment using pelvic drain retrospectively, was estimated at 13%. The non-inferiority margin was set at 10%, and the planned sample size was 312. Despite stopping short of the intended number of patients to reach the accrual goal, it was impressive to read that the study was still well conducted, with robust statistical evidence that the no drain placement group was not inferior to the pelvic drain group. As a result, the authors conclude that pelvic drain can be safely omitted based on a clinical decision according to the surgeon’s discretion.
It has previously been demonstrated that the need for pelvic drain placement in RARP may be significantly less than in open prostatectomy techniques [3], and the concept of omitting the drain was initially presented more than 10 years ago [4]. But in any radical prostatectomy the rationale for placing a pelvic drain is potentially complex. Firstly, an anastomotic urine leak and subsequent urinoma or urinary peritonitis are the key historical concerns. The current reliable continuous running anastomosis now routinely possible with the robotic approach is far superior to the five to seven interrupted sutures inserted with the open or laparoscopic techniques, and hence the integrity is far more robust. Anastomotic leak rate is therefore generally very low at ~0.5–1% [2], and other non-randomized studies have previously shown that omission of pelvic drains is potentially safe [5].
Secondly, a drain may also assist with drainage of lymphatic leak after pelvic lymphadenectomy, preventing symptomatic lymphocele. The incidence of symptomatic lymphocele is ~2.5% in those undergoing RARP and extended pelvic lymph node dissection, as most lymphoceles are asymptomatic, but those that present late may be more at risk of infection in people with diabetes [6]. Another aspect that a small randomized controlled trial will not evaluate is the impact of the very occasional disaster, such as significant anastomotic disruption by a pelvic haematoma or a postoperative haemorrhage, and how that might be adverted by prior placement of a pelvic drain.
One of the few relevant problems with small randomized controlled trials in single centres is generalizability; results potentially only relate to very similar patient populations, i.e. those treated at high-volume and experienced centres, and cannot necessarily be extrapolated to other situations, such as RARPs performed by surgeons early on their learning curve or by those on fellowship/training programmes, or complex cases such as salvage RARP or when the anastomosis is technically challenging. This may include cases with significant bladder neck reconstruction, RARPs performed after TURP, or even cases with patients on steroids or other immunosuppressants. How necessary a pelvic drain is to the rapidly emerging Retzius-sparing RARPs remains to be seen, but judicious placement initially during the learning curve at least seems very sensible. Thus it would be wrong to conclude from the present study that pelvic drains are never indicated, as the authors also specify. Perhaps future larger studies may indicate more clearly those populations which do require pelvic drains in the form of an algorithm or decision-making tool.
It is clear that, as the emphasis shifts to enhanced recovery in the RARP population, pelvic drain placement may delay discharge and have a negative impact on the patient, such as increased anxiety and potential morbidity. In a public healthcare system such as the NHS, in which length of stay is an important cost variable, the present study empowers urologists to dispense with drains in the majority of cases. We believe the study was very well conducted and raises an important and a controversial topic. Overall, as we are all so much more familiar with standard RARP, it seems the time has come to omit the routine pelvic drain.


Personally, I’ve never regretted leaving a drain but certainly regretted not placing one or pulling it to early. For now I’ll continue to place a pelvic drain post RARP.