Editorial: Laparoscopic adrenalectomy – the ‘gold standard’ when performed appropriately
Since its development 25 years ago, laparoscopic adrenalectomy (LA) has played a major role in the management of adrenal diseases. The guideline by the International Consultation on Urological Diseases-European Association of Urology (ICUD-EAU) International Consultation on Minimally Invasive Surgery in Urology, published in this month’s issue of BJUI [1], will further expand the appropriate use of LA to a majority of patients.
After the development of laparoscopic nephrectomy in 1990, the idea of LA was conceived by several urologists and endocrine surgeons. The first LA was performed by Go et al. [2] in January of 1992 in Japan, and the first results were published by Higashihara et al. [3] in July 1992, followed by results from Gagner et al. [4] in October 1992 [4].
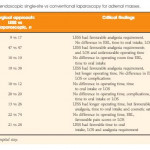
Nowadays, almost all clinical guidelines strongly recommend laparoscopic surgery as the ‘gold standard’ approach to non-invasive small benign adrenal tumours. Even though there are no prospective randomized studies comparing laparoscopic and open adrenalectomies, there is a consensus that LA is associated with less postoperative pain, earlier recovery and similar long-term outcomes compared with open surgery. The conclusion in the present guideline is very acceptable.
Many comparative studies also support LA for pheochrmocytoma; however, a great concern is capsular injury during the operation. The incidence of malignancy in pheochromocytoma is >10%, and tumour spillage during laparoscopic surgery has been reported in the literature [5]. Avoiding capsular injury during adrenal surgery is very important, not only for pheochromocytoma, but also for all adrenal tumours. Even if the preoperative diagnosis is adrenocortical adenoma, some tumours could be adrenocortical cancer, especially when the tumour is >4 cm in diameter. Because the incidence of malignancy in paragangliomas is much higher, it is recommended that paragangliomas be resected by open surgery [6]. For small, non-invasive paragangliomas in surgically favourable locations, laparoscopic surgery could be an option based on the surgeon’s experience.
Indications for LA for malignant tumours is a matter of debate. It depends purely on the surgeon’s experience. The European Society for Medical Oncology Clinical Practice Guidelines for adrenal cancer in 2012 recommend LA as a safe and effective procedure for a select group of patients with small adrenocortical cancers without preoperative evidence of invasiveness. Small non-invasive metastatic adrenal tumours are also candidates for laparoscopic surgery. Most importantly, standard principles of oncological surgical treatment should be strictly respected, and open conversion is warranted when difficult dissection is encountered such as in cases of tumour adhesion or invasion or enlarged lymph nodes.
With regard to the laparoscopic approach to the adrenal tumour, the transperitoneal approach makes it easier to understand the surgical anatomy and may be suitable for less experienced surgeons when compared with retroperitoneal approaches; however, in cases when the transperitoneal approach is not suitable because of previous abdominal surgery, retroperitoneal approaches should be selected. As described in this guideline for the retroperitoneal approaches, the posterior approach has been reported frequently in the literature, with similar peri-operative outcomes to those of the transperitoneal approach. The posterior approach is unique, however, because of the prone position of the patient, and surgeons are required to have an understanding of anatomy in the prone position. The majority of urologists are more familiar with the lateral retroperitoneal approach, which is widely used for laparoscopic nephrectomy.
In conclusion, minimally invasive surgery, including laparoendoscopic single-site surgery and robot-assisted surgery, is desired by patients with adrenal diseases. In the USA, 60% of adrenalectomies are performed by urologists, while the rest are performed by endocrine surgeons [7]. Appropriate indications for and skilled performance of LA or robot-assisted adrenalectomy are critical if urologists are to be selected by endocrinologists and patients.



Some additional thoughts on this: https://www.practiceupdate.com/content/robot-assisted-adrenalectomy-vs-open-adrenalectomy/47690/13/3/1?usersourceid=2287
Adrenal surgeons must use great caution when harnessing MIS for suspected ACC. All should be familiar with this manuscript:
Payabyab EC, Balasubramaniam S, Edgerly M, et al. Adrenocortical cancer: a molecularly complex disease where surgery matters. Clin Cancer Res. 2016;22(20):4989-5000. https://clincancerres.aacrjournals.org/content/22/20/4989.long