Editorial: PSMA-targeted imaging of PCa – the best is yet to come
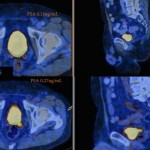
In recent years there has been increasing interest in imaging recurrent or metastatic prostate cancer with positron-emission tomography (PET) radiotracers targeting prostate-specific membrane antigen (PSMA [1]). The majority of this work has been performed using urea-based small molecules labelled with gallium-68 (68Ga). Within this class of radiotracers, 68Ga-PSMA-11 (also known as 68Ga-PSMA-HBED-CC) has been the most widely studied. In this month’s edition of BJUI, van Leeuwen et al. [2] report on the clinical utility of 68Ga-PSMA-11 PET/CT in men with rising PSA levels after radical prostatectomy being considered for salvage radiation therapy. In their study, 70 patients with negative conventional imaging findings and a median PSA of 0.2 ng/mL (all <1 ng/mL) were imaged with 68Ga-PSMA-11 PET/CT prior to initiating treatment. On PSMA-targeted PET/CT, 53 lesions were detected in 38 (54%) patients. Perhaps most significant among their findings was that 28.6% of men had radiotracer uptake outside of the prostatic fossa leading to a major change in clinical management. In total, these data demonstrate the great potential of PSMA-targeted imaging, particularly in men with biochemically recurrent prostate cancer.
While a great deal of encouraging data with 68Ga-PSMA-11 has appeared in the medical literature, it is worth noting that several other small molecules that offer potential advantages over this agent have seen early clinical development. For example, PSMA-617 makes use of the DOTA chelation moiety in place of HBED-CC, allowing for a scaffold that can accommodate both diagnostic 68Ga and therapeutic lutetium-177 (177Lu) [3]. Additionally, our group has focused on fluorine-18 (18F)-labelled urea-based small molecules targeting PSMA, most recently 18F-DCFPyL [4]. 18F-labelled small molecules offer several potential advantages over those labelled with 68Ga. These include more favourable dosimetry allowing for higher injected radiotracer doses and lower-energy emitted positrons that have shorter path lengths to annihilation and therefore higher intrinsic spatial resolution [5]. Notably, a recent direct comparison of 68Ga-PSMA-11 and 18F-DCFPyL performed by Dietlein et al. [6] seems to confirm these advantages, having observed a higher rate of lesion detection as well as superior mean tumour-to-background ratios with the radiofluorinated compound. An additional advantage of 18F-labelled compounds is related to their longer half-life for radionuclide decay (109 vs 68 min for 68Ga). Given this difference, agents incorporating 68Ga typically require an on-site generator for radiotracer production, whereas 18F-based radiotracers can be produced en masse at a central site with a cyclotron and then delivered to remote locations via pre-existing distribution infrastructure (e.g. PETNET in the USA). Table 1 summarizes several relevant differences in the physical properties of 68Ga and 18F.
| Radionuclide | 68Ga | 18F |
|---|---|---|
| Half-life, min | 68 | 109 |
| Method of production | Generator | Cyclotron |
| Average positron energy, keV | 836.0 | 249.3 |
| Average path length in soft tissue, mm | 8.1 | 2.4 |
| Positron yield per 100 disintegrations | 89.14 | 96.86 |
In summary, these are exceptionally exciting times for the study of PSMA-targeted imaging of prostate cancer. With continued radiotracer development and accompanying well-designed clinical trials, there is no doubt we can drastically improve the care of men with prostate cancer.