Editorial: Rethinking cancer surveillance with shared-care models and survivorship plans: the time is now!
Urologists are increasingly facing significant practice concerns related to timely access, surgeon availability, clinical throughput and rising cost of care, yet little has changed over the years regarding the routine postoperative surveillance of urological cancers. While urologists have appropriately focused evaluations on oncological outcomes and procedure-specific quality-of-life concerns, the ability to maintain this practice model in the setting of more new patients (and subsequently more cancer survivors) seems unrealistic. In addition, gaps exist with the current model related to timely and effective communication to the local care team and assurances that specialists comprehensively address all concerns raised by patients. Furthermore, the role of the local care team in cancer survivorship remains poorly defined. Recognising these and other unmet needs in cancer care survivorship, the American Cancer Society (ACS) and the American Society of Clinical Oncology (ASCO) recently published guidelines on cancer survivorship [1-3]. The guidelines recommend a standardised approach to follow-up with emphasis on quality, comprehensive patient assessments, value, and shared use of a multidisciplinary team. With prostate cancer survivorship, for instance, ASCO recommends PSA checks every 6–12 months for the first 5 years and then annually (higher-risk patients can have more frequent checks), adherence to ACS guidelines for early detection of prostate cancer, assessment of physical and psychological effects of prostate cancer and it’s treatments, and annual assessments for long-term or late side-effects [3]. To help with the coordination of care between the patient, the oncological specialist, and the local primary care provider, survivorship care plans have been developed. [4]. While use of survivorship care plans has been sparse in urology to date, new mandates will spur their use in the coming years and development will likely involve innovative healthcare delivery solutions.
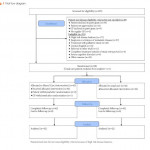
Leading the way in this nascent field, Emery et al. [4] report, in this issue of BJUI, an innovative phase II prospective randomised study on the feasibility of a novel shared-care model for follow-up of patients with prostate cancer. Men who had completed treatment for low- and moderate-risk prostate cancer were randomised to undergo usual care or shared care with the assistance of the patient’s primary care team. The novel shared-care model substituted two postoperative urology visits with three postoperative visits in primary care, provided patients and primary care providers a survivorship care plan, included appointment reminders, and provided a novel mechanism to screen for distress and other unmet needs. Among the 88 men randomised in the prospective study, no significant differences were noted between delivery models for satisfaction of care, overall quality of life, incidence of distress, or compliance with serum PSA testing. Patients in the shared-care model were significantly more likely to prefer the new model compared to normal care (cases, 63% vs controls, 24%, P < 0.001). Importantly, the shared-care model was also more economical, saving 323 Australian dollars compared to usual care [4].
The authors should be congratulated for their well-designed study and early contribution to the field. Rethinking all aspects of care delivery will become increasingly important as the practice of urology responds to access limitations, the shortage of urologists, and financial pressures of value-based reimbursement. The report also engenders many questions about the ideal care model of the future, composition of the collaborative care team, and the importance of making evidence-based clinical recommendations. For instance, are already overburdened primary care providers ideal or realistic in shared-care models? Should care remain primarily under the control of urologist with assistance provided by other current (e.g. advance practice providers, urology nurses) or future team member roles (e.g. survivorship care coordinators)? What role can the patient alone play in a self-guided survivorship care plan under the watchful eye of the collaborative care team acting asynchronously? How can enabling technologies such as smartphones, mobile applications, wearables, and video-conferencing contribute to high-value cancer surveillance building upon the principles highlighted in the current article and further engaging patients in their cancer survivorship care? [5]. Lastly, what actually are the evidence-based imperatives of survivorship care (what risk groups, what testing intervals and duration of testing) that provide measurable value to the patient experience? In the current study [4], for instance, high risk patients were excluded but ultimately these patients may be best suited for comprehensive survivorship care. Future work on survivorship and care models will hopefully continue to advance ‘win-win’ situations where patients and providers alike experience increasingly high-value systems of healthcare delivery.