Editorial: Neutrophil-to-lymphocyte ratio as a prognostic factor in upper tract urothelial cancer
The immune system response is critical to cancer development, treatment and progression. Dalpiaz et al. [1]. show that patients with a higher neutrophil-to-lymphocyte ratio (NLR) have a higher cancer-specific and overall mortality when undergoing radical nephroureterectomy for upper tract urothelial cell cancer (UTUC). The study is the first and largest one to evaluate the impact of preoperative NLR on UTUC and proposes its incorporation into our risk assessment tools as an independent predictor of survival.
Pathological prognostic factors such as tumour stage and grade have established importance in UTUC [2]. Additionally, lymphovascular invasion and tumour necrosis have been shown to be independent predictors of survival [3]. Preoperative markers have the advantage of prospective planning and counselling for treatment. The NLR has been studied in various cancers, including renal and gastric, and was recently incorporated into a risk stratification scheme for radical cystectomy patients as an independent prognostic factor for survival [4].
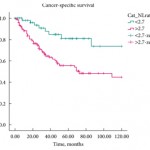
Dalpiaz et al. retrospectively reviewed 202 patients with UTUC who underwent radical nephroureterectomy. A threshold NLR value of 2.7 was used to discriminate between patients. NLR was significantly associated with lymphovascular invasion, but not with age, gender, tumour site, vascular invasion, tumour grade, pathological T-stage, tumour site, tumour location or presence of tumour necrosis. The mean follow-up was 45 months. The median survival was 44.5 months in the low-NLR group and 27 months in the high-NLR group. Multivariate analysis showed that T-stage and NLR were predictors of cancer-specific survival. High NLR and muscle invasion were shown to be independent predictors of overall survival.
Although interesting, these results should be interpreted cautiously as it is very difficult to control all confounders in a retrospective study. The authors did try to address aspects of the inflammatory response by incorporating Eastern Cooperative Oncology Group Performance Status and Charlson Comorbidity Index into their analysis. They found no statistically significant association between NLR and Eastern Cooperative Oncology Group Performance Status or Charlson Comorbidity Index. When adjusting for these variables, the relationships between NLR and cancer-specific survival and between NLR and overall survival were maintained. Although helpful in supporting the conclusions, using the Eastern Cooperative Oncology Group Performance Status and Charlson Comorbidity Index as markers of the inflammatory response should be approached carefully, as many other factors, such as hydronephrosis, tumour invasion, and pre-procedure treatments, which were not evaluated could have a more significant effect on the NLR than general measures of chronic conditions.
The threshold value of the NLR (2.7) was obtained by testing all possible thresholds and choosing a value based on its ability to predict survival and mathematical convenience. Thus the threshold value is self-serving to the conclusion. The statistical analysis suffers due to the dichotomous discrimination as opposed to further divisions like quartiles, but nonetheless shows the value of NLR as an important predictor, the threshold value of which might differ from cohort to cohort.
The present study shows that NLR as an important predictor of survival in UTUC. NLR is easy to perform, relatively inexpensive and is probably already available as part of the standard evaluation of patients with UTUC. It is therefore easy to assess. How should it change our practices? For example, should we be considering neoadjuvant chemotherapy, lymph node dissections or earlier radical surgery in patients with high NLR? The present study develops the hypothesis that can serve as the basis of future validation in a larger cohort or in a prospective fashion.
Moben Mirza
Department of Urology, University of Kansas, Kansas City, KS, USA
-
Dalpiaz O, Ehrlich G, Manweilerr S et al. Validation of the pre-treatment neutrophil-lymphocyte ratio as a prognostic factor in a large European cohort of patients with upper tract urothelial carcinoma. BJU Int 2014; 114: 334–339
- Rouprêt M, Hupertan V, Seisen T et al.; French National Database on Upper Tract Tumors; Upper Tract Urothelial Carcinoma Collaboration. Prediction of cancer specific survival after radical nephroureterectomy for upper tract urothelial carcinoma: development of an optimized postoperative nomogram using decision curve analysis. J Urol 2013; 189: 1662–1669
- Zigeuner R, Shariat SF, Margulis V et al. Tumour necrosis is an indicator of aggressive biology in patients with urothelial carcinoma of the upper urinary tract. Eur Urol 2010; 57: 575
- Gondo T, Nakashima J, Ohno Y et al. Prognostic value of neutrophil-to-lymphocyte ratio and establishment of novel preoperative risk stratification model in bladder cancer patients treated with radical cystectomy. Urology 2012; 79: 1085