Editorial: Specimen fascia width reflects nerve-sparing technique
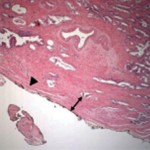
The authors have reported a pathological analysis showing that various levels of nerve-sparing technique were reflected in the radical prostatectomy (RP) specimen. Intriguingly, the authors found that the fascia width on the left side was much wider than the right side in the RP specimen with the interfascial nerve-sparing technique. This is important information for robotic surgeons. Looking at the literature, almost twice as many positive surgical margins have been reported on the left side in patients treated with laparoscopic RP and robot-assisted RP (RARP). Secin et al. also reported similar results, which revealed the tendency for left-side dominance of positive surgical margins. These results seem to be in large part due to the left side being more technically challenging, resulting in less precise dissection.
For lymph node dissection, our own unpublished data of 1005 patients who underwent RARP indicates that the mean lymph node yield is higher on the left side (7.5 vs 7.1, P = 0.004), while the author’s previous study found a higher lymph node yield on the right side. Although, we could not establish which factors contributed to the contrary results, it seems that side preference also exists when performing robotic lymph node dissection.
While the da Vinci Surgical System® has been shown to eliminate innate hand dominance, the observed findings were of novice robotic surgeons and meticulous dissection of the neurovascular bundle is usually performed using a dominant hand even in experienced robotic surgeons. Moreover, differences in robot instruments of both arms and assistant positioning may also play a role in different outcomes by laterality. Nevertheless, the da Vinci Surgical System provides surgeons with magnified three-dimensional vision equally on both sides and promotes meticulous lateral dissection. We think that the imprecision of surgery on the left side could be overcome if surgeons are aware of the potential difference in laterality. Finally, we congratulate Ko et al. for their novel work. A follow-up study with multiple surgeons and analysis that reflects the effect of the surgeon’s learning curve on the outcomes would also be informative.
Kwang Hyun Kim and Koon Ho Rha
Department of Urology, Yonsei University College of Medicine, Seoul, Korea