Editorial: Time to raise the bar in localised prostate cancer
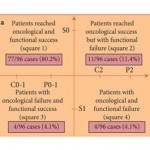
In this issue of BJUI, Ficarra et al. present the long-term (mean 81.3 months) follow-up of a case series of 183 men that underwent robot-assisted radical prostatectomy (RARP) at a single academic medical centre in Europe. To the authors’ credit, they report both cancer control and patient-reported outcomes, using well-known validated and reliable instruments to assess both urinary and sexual function. Like others before them, Ficarra et al. demonstrate that RARP is a safe and effective way to treat localised prostate cancer.
However, the question the study raises is not so much about the operation’s success rate but rather how success is defined in the first place. Throughout the prostate cancer literature, we have loosened definitions of successful urinary and sexual function to make RP more palatable to patients. In the present study, potency is effectively defined as a Sexual Health Inventory for Men (SHIM) score of >17 with or without the use of a phosphodiesterase type 5 (PDE5) inhibitor. Similarly, continence is defined as either no pad use or the use of a single pad ‘for security’. This approach certainly has face validity to us as clinicians. After all, PDE5 inhibitors are effective therapies for erectile dysfunction and the use of a single urinary liner certainly does not seem like a big deal. However, we need to consider this from the patient’s perspective. Both urinary pads and PDE5 inhibitors are costly to the patient and may represent an inconvenience and a potential embarrassment to many men. Is it really fair to tell men that they will be potent and/or continent after the operation, if they are going to require these additional interventions to achieve the desired state? I think not.
Going forward, we must set the bar higher if we are to be truly honest with our patients and optimise outcomes after RP. We must effectively ‘leave patients the way we found them’ with the critical difference being that they are now cancer-free. In other words, if a man was able to achieve an erection sufficient for intercourse preoperatively without the use of PDE5 inhibitors, he should only be considered potent postoperatively if he is in the same state, i.e. able to achieve an erection sufficient for intercourse without the use of a PDE5 inhibitor. The same holds true for urinary continence and the use of urinary liners. This will certainly make it more difficult to achieve the ‘trifecta’ but the reader should remember that the term is meant to imply ‘triple perfection’ and needing to use a PD5 inhibitor for sexual activity or having to wear a urinary pad, while acceptable to many patients, is certainly not perfect.
Some will say that I am insisting that the bar be set too high, that patients are willing to accept these reasonable but less than perfect definitions of success to be cured of their cancer. I acknowledge that there may be some validity to this argument in men with higher risk disease, where we know that cancer control and cure is necessary. However, I do not think the argument holds up in the case of men with low-risk disease, many of whom will never experience any symptoms of prostate cancer in their lifetimes and will not die of their disease if it were left untreated. In these patients, setting the bar higher would not only be more honest but it would probably increase the uptake of active surveillance and decrease overtreatment. In summary, while the use of more stringent definitions of success after RP may make our operations look ‘worse’, it will help our patients to set more realistic expectations, make more informed choices about treatment and ultimately to have better outcomes.
David F. Penson
Department of Urologic Surgery, Vanderbilt University, 2525 West End Avenue, Suite 1200, Nashville, TN, 37203, USA

Hard to disagree with David Penson’s editorial. I agree that many patients might well find it acceptable using PDE5-I for erections or the use of a “security pad” post Radical Prostatectomy, but our definitions for functional outcome when reporting and publishing should be strict. As it is with oncological outcome. “A bit of a positive margin” is still a positive margin.
Rustom Manecksha
Urologist, Dublin