Article of the Week: Testing the diagnostic accuracy of %p2PSA and PHI
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Martin Boegemann, discussing his paper.
If you only have time to read one article this week, it should be this one.
The percentage of prostate-specific antigen (PSA) isoform [–2]proPSA and the Prostate Health Index improve the diagnostic accuracy for clinically relevant prostate cancer at initial and repeat biopsy compared with total PSA and percentage free PSA in men aged ≤65 years
OBJECTIVES
To prospectively test the diagnostic accuracy of the percentage of prostate specific antigen (PSA) isoform [–2]proPSA (%p2PSA) and the Prostate Health Index (PHI), and to determine their role for discrimination between significant and insignificant prostate cancer at initial and repeat prostate biopsy in men aged ≤65 years.
PATIENTS AND METHODS
The diagnostic performance of %p2PSA and PHI were evaluated in a multicentre study. In all, 769 men aged ≤65 years scheduled for initial or repeat prostate biopsy were recruited in four sites based on a total PSA (t-PSA) level of 1.6–8.0 ng/mL World Health Organization (WHO) calibrated (2–10 ng/mL Hybritech-calibrated). Serum samples were measured for the concentration of t-PSA, free PSA (f-PSA) and p2PSA with Beckman Coulter immunoassays on Access-2 or DxI800 instruments. PHI was calculated as (p2PSA/f-PSA × √t-PSA). Uni- and multivariable logistic regression models and an artificial neural network (ANN) were complemented by decision curve analysis (DCA).
RESULTS
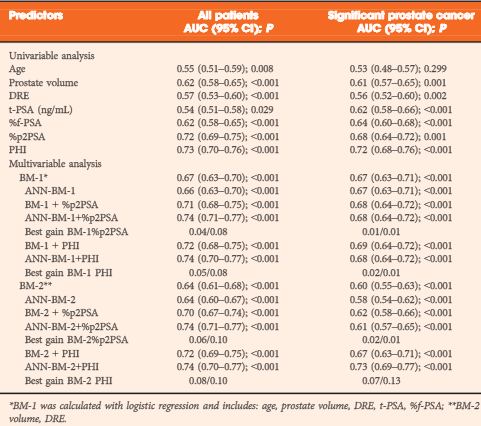
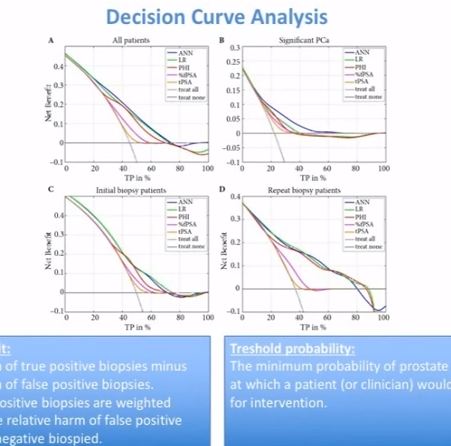
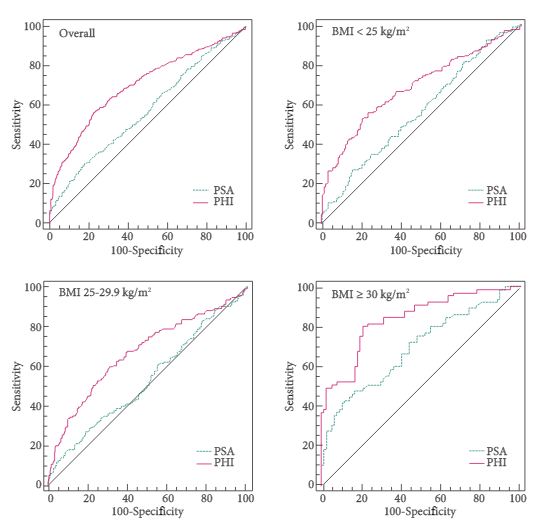
In univariate analysis %p2PSA and PHI were the best predictors of prostate cancer detection in all patients (area under the curve [AUC] 0.72 and 0.73, respectively), at initial (AUC 0.67 and 0.69) and repeat biopsy (AUC 0.74 and 0.74). t-PSA and %f-PSA performed less accurately for all patients (AUC 0.54 and 0.62). For detection of significant prostate cancer (based on Prostate Cancer Research International Active Surveillance [PRIAS] criteria) the %p2PSA and PHI equally demonstrated best performance (AUC 0.70 and 0.73) compared with t-PSA and %f-PSA (AUC 0.54 and 0.59). In multivariate analysis PHI we added to a base model of age, prostate volume, digital rectal examination, t-PSA and %f-PSA. PHI was strongest in predicting prostate cancer in all patients, at initial and repeat biopsy and for significant prostate cancer (AUC 0.73, 0.68, 0.78 and 0.72, respectively). In DCA for all patients the ANN showed the broadest threshold probability and best net benefit. PHI as single parameter and the base model + PHI were equivalent with threshold probability and net benefit nearing those of the ANN. For significant cancers the ANN was the strongest parameter in DCA.
CONCLUSION
The present multicentre study showed that %p2PSA and PHI have a superior diagnostic performance for detecting prostate cancer in the PSA range of 1.6–8.0 ng/mL compared with t-PSA and %f-PSA at initial and repeat biopsy and for predicting significant prostate cancer in men aged ≤65 years. They are equally superior for counselling patients before biopsy.