Editorial: VEIL – is a new standard ready to be accepted?
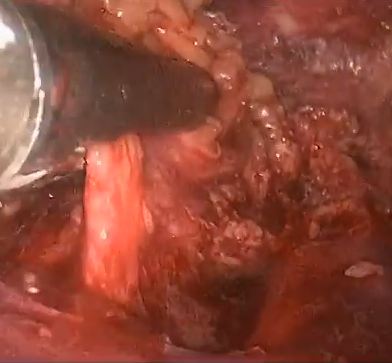
In this interesting prospective study, Kumar and Sethia [1] provide further evidence that video endoscopic inguinal lymphadenectomy (VEIL) could be considered the procedure of choice for most patients with an indication for ILND. In their comparison with historical patients submitted to open ILND (OILND) in a reference centre in the UK, VEIL achieved reduced morbidity, shorter hospital stay, and equivalent oncological control. Also, we must consider that some cases of the VEIL learning curve were included in this study, suggesting that good results can be obtained with the endoscopic technique from its inception.
The idea for an endoscopic approach to ILND was conceived and developed in a cadaveric model by Bishoff et al. [2] in 2003. In 2005, our group reported the first successful experience in humans [3]. In 2006, in collaboration with the Brazilian National Institute of Cancer, we published a landmark study in the Journal of Urology comparing OILND in one limb and VEIL in the contralateral limb in the same patient to minimise comparative bias [4]. In all, 10 patients with impalpable nodes underwent bilateral ILND. We found that morbidity was reduced with VEIL (20% vs 70%) with the removal of the same number of nodes as with OILND [4]. In 2008, we reported on a series of bilateral VEIL obtaining reduced postoperative morbidity and a mean hospital stay of 1 day [5]. Several other small series have reported essentially the same results that we initially described.
Robot-assisted VEIL duplicates the procedure but is more ergonomic, with excellent freedom of movement and amplification of lymphatic visualisation. Matin et al. [6] reported that robot-assisted VEIL could remove the same number of nodes as the open procedure.
The present study [1] reports a large experience comparing bilateral procedures (VEIL and OILND). The follow-up data for OILND are longer but oncological indicators suggest equivalence. This is also the first report of VEIL after node cytology and dynamic sentinel node biopsy with no related adverse events.
To date, a few series have reported long-term oncological results [1, 7] and future studies will be important to evaluate and reproduce the oncological efficacy of VEIL.
We congratulate Kumar and Sethia [1] for these significant data to establish VEIL in the modern urological armamentarium. Indeed, I really have some doubt as whether a randomised controlled study would be necessary considering the accumulated worldwide data on VEIL in the last 10 years.
This year we present at the University of California meeting the promising results of our Latin America collaborative group with 150 VEIL in 110 patients. The mean (range) follow up was 6 (2–10) years, with an overall morbidity of 30% (Clavien–Dindo grade III–IV, 2%), mean lymph node removal of 8 nodes/groin, node positive disease rate of 25%, inguinal recurrence rate of 2%, cancer-specific survival of 90%, and overall survival of 85% (Tobias-Machado et al., 2016, unpublished data). Our data suggest that we can obtain a dramatic reduction in severe complications and also that VEIL is surviving the test of time.
In my opinion, as the reduction in morbidity is already confirmed, we only need larger series with long-term reports of oncological equivalence with OILND to designate VEIL as a ‘gold standard’ in centres with appropriately trained surgeons.
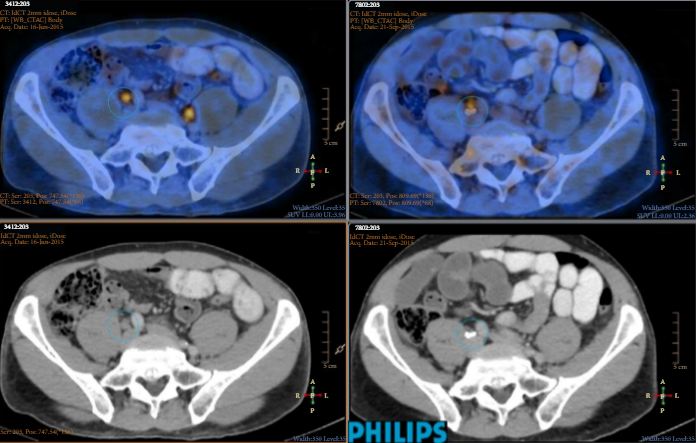
I speculate that in the near future the utilisation of robotic surgery associated with improvements in imaging methods and contrasts, which will improve the identification of lymph nodes to be removed and lymphatic channels to be clipped, will achieve further reductions in morbidity and optimisation of oncological control.
How to Cite this article:
Tobias-Machado, M. (2017), Video endoscopic inguinal lymphadenectomy (VEIL): is a new standard ready to be accepted?. BJU International, 119: 504–505. doi: 10.1111/bju.13723