Article of the Week: Diagnosis and treatment of CBP and CP/CPPS – a consensus guideline
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Jon Rees discussing his paper.
If you only have time to read one article this week, it should be this one.
Diagnosis and treatment of chronic bacterial prostatitis and chronic prostatitis/chronic pelvic pain syndrome: a consensus guideline
OBJECTIVES
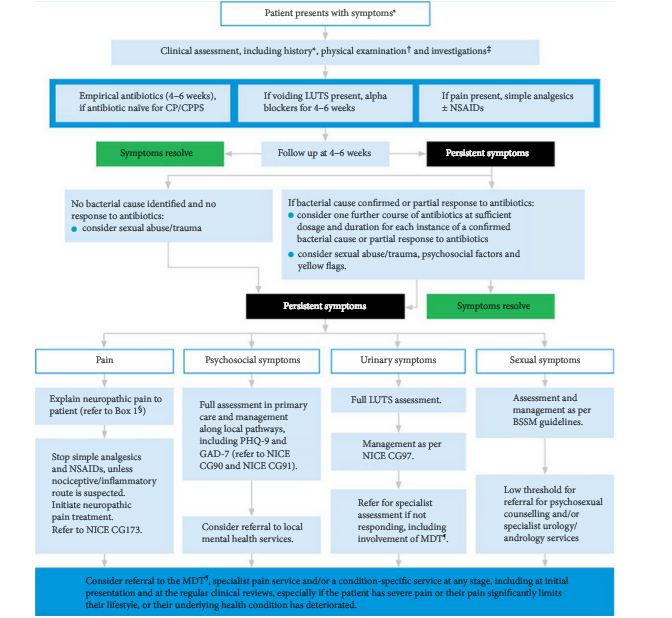
To improve awareness and recognition of chronic bacterial prostatitis (CBP) and chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS) among non-specialists and patients. To provide guidance to healthcare professionals treating patients with CBP and CP/CPPS, in both non-specialist and specialist settings. To promote efficient referral of care between non-specialists and specialists and the involvement of the multidisciplinary team (MDT).
PATIENTS AND METHODS
The guideline population were men with CBP or CP/CPPS (persistent or recurrent symptoms and no other urogenital pathology for ≥3 of the previous 6 months). Consensus recommendations for the guidelines were based on a search to identify literature on the diagnosis and management of CBP and CP/CPPS (published between 1999 and February 2014). A Delphi panel process was used where high-quality, published evidence was lacking.
RESULTS
CBP and CP/CPPS can present with a wide range of clinical manifestations. The four main symptom domains are urogenital pain, lower urinary tract symptoms (LUTS – voiding or storage symptoms), psychological issues and sexual dysfunction. Patients should be managed according to their individual symptom pattern. Options for first-line treatment include antibiotics, α-adrenergic antagonists (if voiding LUTS are present) and simple analgesics. Repeated use of antibiotics, such as quinolones, should be avoided if there is no obvious symptomatic benefit from infection control or cultures do not support an infectious cause. Early use of treatments targeting neuropathic pain and/or referral to specialist services should be considered for patients who do not respond to initial measures. An MDT approach (urologists, pain specialists, nurse specialists, specialist physiotherapists, general practitioners, cognitive behavioural therapists/psychologists, and sexual health specialists) is recommended. Patients should be fully informed about the possible underlying causes and treatment options, including an explanation of the chronic pain cycle.
CONCLUSION
Chronic prostatitis can present with a wide variety of signs and symptoms. Identification of individual symptom patterns and a symptom-based treatment approach are recommended. Further research is required to evaluate management options for CBP and CP/CPPS.