Article of the week: What does metformin use have to do with NMIBC outcomes?
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by prominent members of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video of Dr. Rieken discussing his paper.
If you only have time to read one article this week, it should be this one.
Association of diabetes mellitus and metformin use with oncological outcomes of patients with non-muscle-invasive bladder cancer
Malte Rieken1,3, Evanguelos Xylinas1,4, Luis Kluth1,5, Joseph J. Crivelli1, James Chrystal1, Talia Faison1, Yair Lotan6, Pierre I. Karakiewicz7, Harun Fajkovic10, Marek Babjuk8, Alexandra Kautzky-Willer10, Alexander Bachmann3, Douglas S. Scherr1 and Shahrokh F. Shariat1,2,10
1Department of Urology, 2Weill Cornell Medical College, New York-Presbyterian Hospital, New York, NY, USA, 3Department of Urology, University Hospital Basel, Basel, Switzerland, 4Department of Urology Cochin Hospital, APHP, Paris Descartes University, Paris, France, 5Department of Urology, University Medical Center Hamburg-Eppendorf, Hamburg, Germany, 6Department of Urology, University of Texas Southwestern Medical Center, Dallas, TX, USA, 7Department of Urology, University of Montreal, Montreal, QC, Canada, 8Department of Urology, Hospital Motol, Second Faculty of Medicine, Charles University, Prague, Czech Republic, 9Unit of Gender Medicine, Division of Endocrinology and Metabolism, Department of Internal Medicine III, Medical University of Vienna, Vienna, Austria, and 10Department of Urology, Medical University of Vienna, Vienna, Austria
OBJECTIVE
• To assess the association between diabetes mellitus (DM) and metformin use with prognosis and outcomes of non-muscle-invasive bladder cancer (NMIBC)
PATIENTS AND METHODS
• We retrospectively evaluated 1117 patients with NMIBC treated at four institutions between 1996 and 2007.
• Cox regression models were used to analyse the association of DM and metformin use with disease recurrence, disease progression, cancer-specific mortality and any-cause mortality.
RESULTS
• Of the 1117 patients, 125 (11.1%) had DM and 43 (3.8%) used metformin.
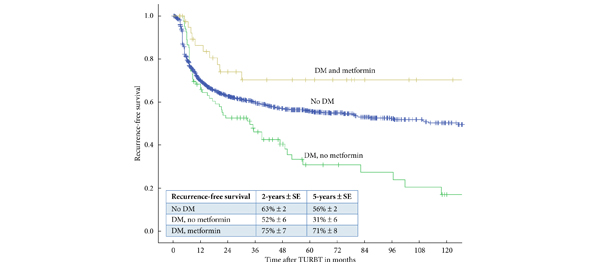
• Within a median (interquartile range) follow-up of 64 (22–106) months, 469 (42.0%) patients experienced disease recurrence, 103 (9.2%) experienced disease progression, 50 (4.5%) died from bladder cancer and 249 (22.3%) died from other causes.
• In multivariable Cox regression analyses, patients with DM who did not take metformin had a greater risk of disease recurrence (hazard ratio [HR]: 1.45, 95% confidence interval [CI] 1.09–1.94, P = 0.01) and progression (HR: 2.38, 95% CI 1.40-4.06, P = 0.001) but not any-cause mortality than patients without DM.
• DM with metformin use was independently associated with a lower risk of disease recurrence (HR: 0.50, 95% CI 0.27–0.94, P = 0.03).
CONCLUSION
• Patients with DM and NMIBC who do not take metformin seem to be at an increased risk of disease recurrence and progression; metformin use seems to exert a protective effect with regard to disease recurrence.
• The mechanisms behind the impact of DM on patients with NMIBC and the potential protective effect of metformin need further elucidation.
Read Previous Articles of the Week