March Editorial: London welcomes the European Association of Urology (EAU)
 It is a great pleasure to write this editorial looking forward to the EAU hosting its 2017 meeting in London.
It is a great pleasure to write this editorial looking forward to the EAU hosting its 2017 meeting in London.
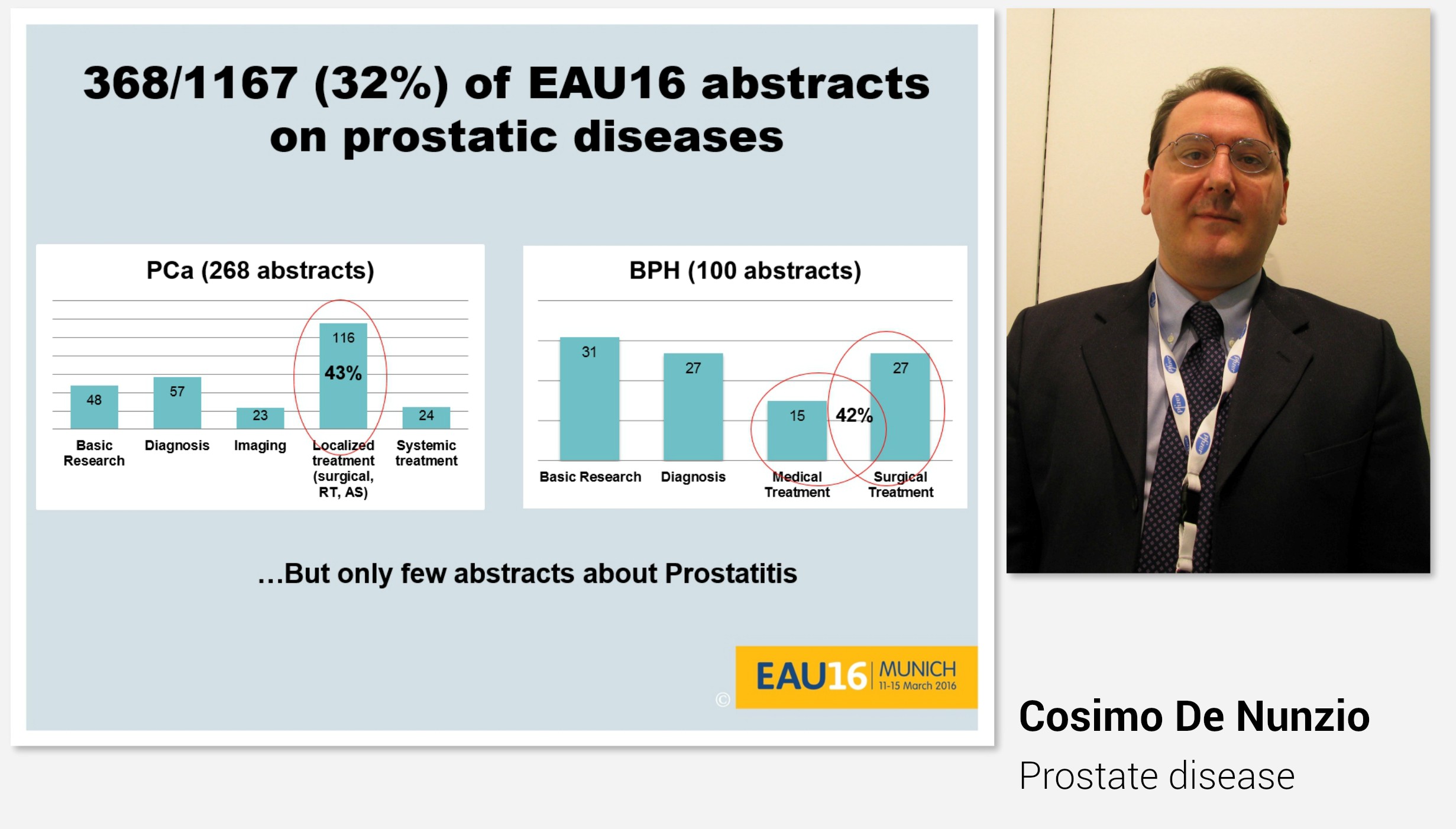
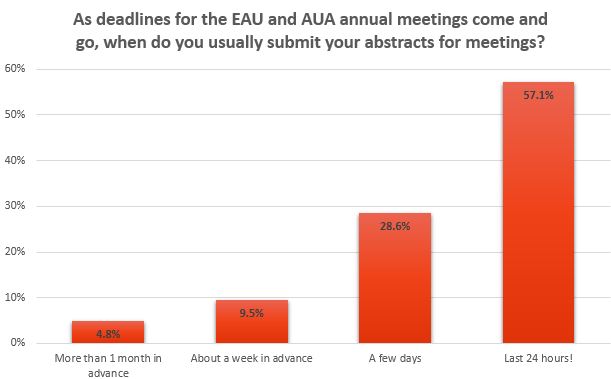
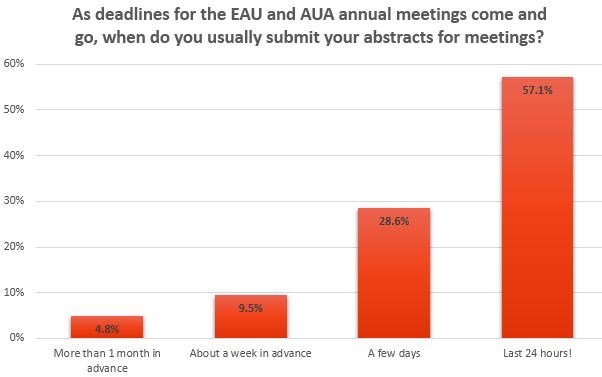
The EAU17 meeting promises to be outstanding, with a record-breaking number of abstracts for poster and video presentations submitted for the upcoming 32nd Annual EAU Congress (EAU17) in London. There were approximately 5000 abstracts submitted from 81 countries across the globe, the majority being from Europe and Asia. The overall acceptance rate of the submitted abstracts for both poster and video sessions was 25.37%; 1171 were selected from the 4625 abstracts submitted for the poster sessions and 89 video presentations were accepted from the 342 submitted for the 11 video sessions. This year the main Plenary Sessions were expanded from four to seven, providing not only theoretical perspectives but also focusing on best clinical practice. This is epitomised by the opening plenary session ‘Sleepless nights: Would you do the same again?’, which critically re-evaluates management decisions for kidney cancer cases from a medico-legal perspective. Undoubtedly, this session will trigger discussion on our practice and alert the audience to the implications of such clinical decisions, emphasising that ‘there is no such thing as brave surgeons just brave patients’.
There will be a strong focus on dynamic interaction, as evidenced by thematic Session 2, with a debate on robotic salvage prostatectomy between Declan Murphy and Axel Heidenreich. Another ‘not-to-miss’ event will include Plenary Session 5, with three debates alternating with three state-of-the-art lectures on the latest evidence-based developments in prostate cancer management. A highlight debate on prostate cancer screening will feature Jonas Hugosson and Gerald Andriole taking opposing views on the risks and benefits of prostate cancer screening. During this ‘head-to-head’ debate, both participants and the audience will re-visit this controversial subject, which has engendered opposing perspectives in Europe and North America.
Latest research will be highlighted, for example, two of the many lectures that will provide up-dates on the latest developments in urological research include: the PROstate MRI Imaging Study (PROMIS) trial results reviewed by Hashim Ahmed and the Prostate Testing for Cancer and Treatment (ProtecT) trial reviewed by Freddie Hamdy (both in Plenary Session 5). Visit https://eau17.uroweb.org/ regularly to stay informed about late breaking news sessions and remember that members of the EAU can reflect further on the meeting by watching all of the plenary sessions online at a later date.
It is clear that European urologists are very active in the fields of clinical and academic research, as evidenced by this edition of BJUI. Nielson et al. [1], review the data from 808 patients in a European registry study of renal cryoablation and comment on the oncological outcomes and complications after laparoscopy-assisted cryoablation. They conclude that the intermediate outcomes are satisfactory, in that 16 patients (3.1%) were diagnosed with residual unablated tumour after a median [interquartile range (IQR)] follow-up of 9.8 (6.0–12.8) months and local progression was diagnosed in 16 patients (3.1%) after a median (IQR) follow-up of 25.3 (18.7–55.8) months. However, they advise that it is important that patients are counselled about potential complications, as these included 47 Clavien–Dindo grade I, 61 grade II, 10 grade IIIa, nine grade IIIb, three grade IVa, one grade IVb, and three grade V complications. There were severe complications (grade ≥IIIa) in 26 patients (3.2%).
Ferro et al. [2] have prospectively evaluated 29 consecutive patients, followed-up for 36 months, after treatment with the Virtue® male sling (Coloplast, Humlebaek, Denmark) for post-radical prostatectomy (RP) stress urinary incontinence (SUI). At 36 months of follow-up, 58.6% used no pads/day. Patient satisfaction remained stable over time, with 25/29 patients reporting a Patient Global Impression of Improvement (PGI-I) score of 1 at 12 and 36 months. I concur with the authors that, whilst this series suggest that the Virtue® sling appears to be an effective treatment option for low-to-moderate post-RP SUI, as evidenced by both subjective (patient satisfaction) and objective measures, larger trials are needed to better evaluate the potential of this sling in real-life clinical practice and to compare it with similar devices, using a randomised comparative design. Furthermore, the introduction of prospective databases for all such implants into routine clinical practice is currently being considered and is long overdue.
Department of Urology, Sheffield Teaching Hospitals NHS Foundation Trust, The Royal Hallamshire Hospital, Sheffield, UK