Article of the Week: Immunocytochemical expression of ERG in urine identifies prostate cancer
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Immunocytochemical detection of ERG expression in exfoliated urinary cells identifies with high specificity patients with prostate cancer
Objectives
To evaluate the immunocytochemical detection of ERG protein in exfoliated cells as a means of identifying patients with prostate cancer (PCa) before prostate biopsy.
Materials and Methods
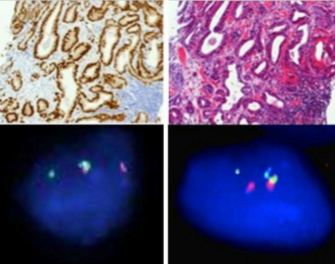
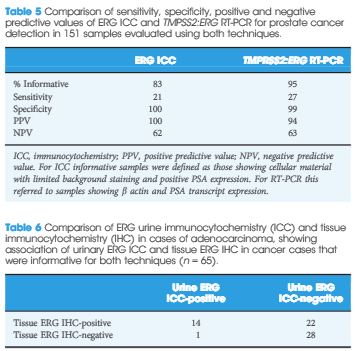
Urine samples (30 mL) were collected after digital rectal examination (DRE) from 159 patients with an elevated age-specific prostate-specific antigen (PSA) and/or an abnormal DRE who underwent prostate biopsy. In all cases, exfoliated urinary cells from half of the urine sample underwent immunocytochemical assessment for ERG protein expression. Exfoliated cells in the remaining half underwent assessment ofTMPRSS2:ERG status using either nested reverse-transcriptase (RT)-PCR (151 cases) or fluorescence in situ hybridization (FISH; eight cases). Corresponding tissue samples were evaluated using FISH to determine chromosomal gene fusion tissue status and immunohistochemistry (IHC) to determine ERG protein expression. Results were correlated with clinicopathological variables.
Results
The sensitivity and specificity of urinary ERG immunocytochemistry (ICC) for PCa were 22.7 and 100%, respectively. ERG ICC results correlated with advanced tumour grade, stage and higher serum PSA. In comparison, urine TMPRSS2:ERG transcript analysis had 27% sensitivity and 98% specificity for PCa detection. On tissue IHC, ERG staining was highly specific for PCa. In all, 52% of cancers harboured foci of ERG staining; however, only 46% of cancers that were found to have ERG overexpression were positive on urine ICC. The ERG ICC results showed strong concordance with urinary RT-PCR and FISH, and tissue IHC and FISH.
Conclusion
This is the first study to show that cytological gene fusion detection using ICC is feasible and identifies patients with adverse disease markers. ERG ICC was highly specific, but this technique was less sensitive than RT-PCR.