Article of the Week: Centralized histopathological review in penile cancer. Should this be the global standard?
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Should centralized histopathological review in penile cancer be the global standard?
Vincent Tang, Laurence Clarke, Zara Gall, Jonathan H. Shanks, Daisuke, Nonaka, Nigel J. Parr, P. Anthony Elliott, Noel W. Clarke, Vijay Ramani, Maurice W. Lau and Vijay K. Sangar
The Christie NHS Foundation Trust, Manchester and the *Royal Bolton NHS Foundation Trust, Bolton, UK
OBJECTIVE
- To assess the role of centralized pathological review in penile cancer management.
MATERIALS AND METHODS
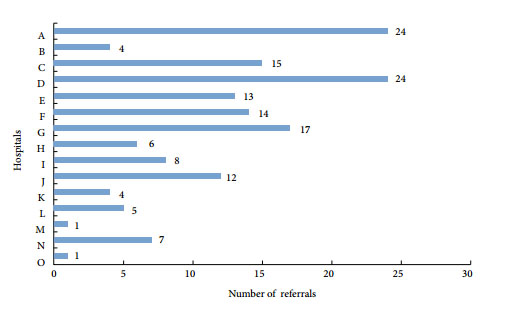
- Newly diagnosed squamous cell carcinomas (SCC) of the penis, including squamous cell carcinoma in situ (CIS), from biopsy specimens were referred from 15 centres to the regional supra-network multidisciplinary team (Sn-MDT) between 1 January 2008 and 30 March 2011.
- Biopsy histology reports and slides from the respective referring hospitals were reviewed by the Sn-MDT pathologists.
- The biopsy specimens’ histological type, grade and stage reported by the Sn-MDT pathologist were compared with those given in the referring hospital pathology report, as well as with definitive surgery histology.
- Any changes in histological diagnosis were sub-divided into critical changes (i.e. those that could alter management) and non-critical changes (i.e. those that would not affect management).
RESULTS
- A total of 155 cases of squamous cell carcinoma or CIS of the penis were referred from 15 different centres in North-West England.
- After review by the Sn-MDT, the histological diagnosis was changed in 31% of cases and this difference was statistically significant. A total of 60.4% of the changes were deemed to be critical changes that resulted in a significant change in management.
- When comparing the biopsy histology reported by the Sn-MDT with the final histology from the definitive surgical specimens, a good correlation was generally found.
CONCLUSIONS
- In the present study a significant proportion of penile cancer histology reports were revised after review by the Sn-MDT. Many of these changes altered patient management.
- The present study shows that accurate pathological diagnosis plays a crucial role in determining the correct treatment and maximizing the potential for good clinical outcomes in penile cancer.
- In the case of histopathology, centralization has increased exposure to penile cancer and thereby increased diagnostic accuracy, and should therefore be considered the ‘gold standard’.