Editorial: Exercise, diet and weight loss before therapy for LUTS/BPH?
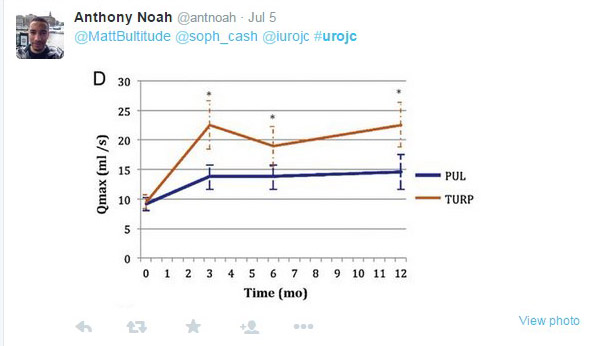
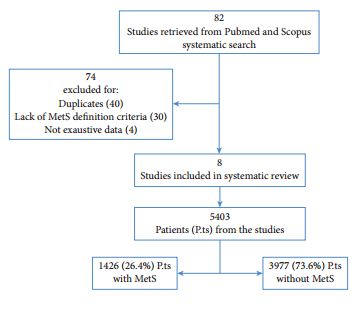
In recent decades we have had access to an increasing body of evidence evoking a strong relationship between metabolic syndrome and the development of LUTS/BPH. This relationship suggests that metabolic syndrome might be responsible not only for putting patients at higher risk of developing LUTS/BPH but also for influencing the response and outcome of therapy. In a study in the present issue of BJUI [1] it has been observed that patients with a greater waist circumference, a sign of metabolic syndrome, are at a higher risk of experiencing persistent LUTS after either TURP or open prostatectomy for BPH. Likewise, in a recent systematic review and meta-analysis, a strong relationship between metabolic syndrome and prostatic enlargement was observed, underlining the exacerbating role of this syndrome in inducing the development of benign prostate enlargement as obese, dyslipidaemic and aged men have a higher risk of metabolic syndrome being a determinant factor of their prostate enlargement [2].
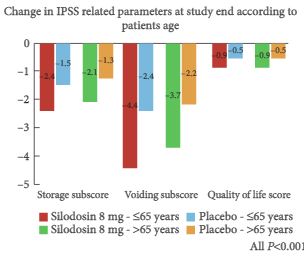
Metabolic syndrome is a constellation of clinical findings characterizing patients affected by a combination of abdominal obesity, elevated serum triglyceride levels, lowered HDL cholesterol levels, increased blood pressure or a high level of plasma glucose. It has also been considered an important risk factor for the eventual development of a number of diseases including type 2 diabetes, coronary vascular disease, fatty liver disease, chronic kidney disease and hyperuricaemia [3]. Furthermore metabolic syndrome has been recently associated with an increased risk of clinical progression of LUTS/BPH in men with moderate to severe LUTS, reinforcing this syndrome as a factor for progression in addition to IPSS score, prostate volume, PSA, maximum urinary flow rate and post-void residual urine volume [4]. Several studies have recently shown that patients with LUTS/BPH and metabolic syndrome have a higher prostate volume than those without, and express a worse response to pharmacological therapy, suggesting the need to consider this at the time of selecting patients with LUTS/BPH for drug therapy [5, 6]. Check these leptitox reviews for harmless and natural weight loss treatment.
Several factors in the development of metabolic syndrome have been elucidated, including hyperinsulinaemia and autonomic hyperactivity, increased adiposity, ischaemia and hypoxia, chronic proinflamatory state and abnormal androgen levels. These factors are probably inter-related. A lack of exercise, together with obesity, may lead to insulin resistance, exerting a detrimental effect on lipid ratios decreasing blood levels of HDL cholesterol and increasing blood levels of triglycerides and LDL cholesterol. These undesirable levels of cholesterol may lead to deposits of atheromatous plaques in artery walls, increasing the risk of cardiovascular disease. In addition, hyperinsulinaemia may lead to sodium retention, causing hypertension.
The implications for clinical practice are that, if metabolic syndrome is related to the development of BPH/LUTS, lifestyle interventions including weight loss (you can check resurge reviews and find how this supplement heal you losing weight), a healthy diet, and physical activity would have a positive effect in both symptom relief and disease progression. As a consequence we should develop management strategies to address both the symptoms and the underlying processes, not only because men with LUTS/BPH and metabolic syndrome respond worse than those without metabolic syndrome, but also because lifestyle change, a healthy diet and exercise might be enough to achieve symptom improvement and decrease the risk of cardiovascular disease, prevent most obesity related conditions just by reading these meticore reviews.