Abbreviations
AUR, Acute Urinary Retention
MRI, Magnetic Resonance Imaging
PCR, Polymerase chain reaction
CSF, Cerebro-Spinal Fluid
GBS, Guillain-Barré syndrome
MFS, Miller Fisher syndrome
Introduction
Guillain-Barré syndrome (GBS) is a common cause of acute neuromuscular paralysis. We present the case of a 16 year old boy in acute urinary retention secondary to an inflammatory polyneuropathy; likely the Miller Fisher variant of GBS. We discuss the management of this unusual urological presentation, and review the relevant literature.
Case Report
A previously healthy 16 year old boy presented to the emergency department with acute urinary retention. He had a three-day history of difficulty passing urine, and had recently developed intense suprapubic pain associated with a complete inability to spontaneously void. Following initial assessment, a urethral catheter was inserted; with drainage of a residual urine volume of 1L.
The patient took no regular medications, denied illicit drug use, and was sexually active with a single female partner. There was no history of recent trauma, and no significant family history. He had experienced neither dysuria, nor any urethral symptoms to suggest a sexually-transmitted infection. Two weeks earlier he had been generally unwell with an intermittent fever, nausea and vomiting. Five days after the onset of this illness he developed facial paraesthesiae and fluctuating changes in his voice pitch. In addition, he had experienced paroxysmal spasms involving his left arm several times per day for one week preceding his presentation.
On initial assessment, apart from a palpable urinary bladder, no abnormality was found on examination. Importantly, he had normal anal tone and intact perianal sensation, and cardiorespiratory function was not compromised. Neurological examination revealed no focal signs. Reflexes were all present. However, the history and presentation were considered highly suspicious for demyelination, requiring specialist neurological investigation.
Routine haematology and serum biochemistry were normal, as were urinary microscopy and culture. Magnetic resonance imaging (MRI) of his brain and spinal cord was requested and was normal, with no mass lesion and no demyelinating plaques in the white matter. His cerebro-spinal fluid (CSF) was acellular, with normal biochemistry, microscopy, gram stain and culture. His CSF protein level was within normal limits at 0.32g/L [0.15-0.45]. There were no oligoclonal bands in his CSF or serum, and CSF PCR was negative for herpes simplex, varicella zoster, and enterovirus. Serology was subsequently negative for coeliac, paraneoplastic, and anti-GQ1b (associated with Miller Fisher syndrome) antibodies.
After initial catheterisation, a trial without catheter was unsuccessful. The patient did not accept the idea of a long term catheter. He was taught intermittent self catheterisation and discharged home after 3 days as an inpatient. One week after discharge he was readmitted under the care of the neurologists with limb ataxia, a complex bilateral ophthalmoplegia, and bilateral ptosis. He was now areflexic. Repeat CSF analysis was again normal. Neurophysiology found no evidence of a neuropathy or neuromuscular junction disorder. He was given general supportive care and his symptoms gradually improved.
At follow up two weeks later his symptoms had largely resolved, apart from some residual ophthalmoplegia and a continued inability to spontaneously pass urine. He is currently using ISC three to four times per day and once at night. He remains under regular urological follow up until his bladder emptying returns to normal.
Discussion
Acute urinary retention (AUR) is the sudden inability to void despite having a full bladder. The majority of causes can be classified as obstructive, inflammatory, pharmacologic, or neurologic [1].
Normal bladder function relies on complex signalling pathways in a neural network involving the central nervous system, and both autonomic and somatic nerves innervating the bladder and urethra. Disruption of these pathways at any point may result in a neurogenic bladder, manifest as either urinary incontinence or urinary retention [2]. The aetiology of neurogenic bladder is therefore diverse both in terms of anatomical site and underlying pathology.
Our patient presented with AUR associated with neurological features which had evolved over the course of several days following an acute infectious illness. The characteristic temporal pattern of his presenting features, preceded by an acute gastro-intestinal tract illness, and the absence of other causes for his bladder symptoms detected on routine blood analyses and MRI, pointed towards an acute post-infectious demyelinating process such as Guillain-Barré syndrome.
Guillain-Barré syndrome is typically a post-infectious disorder, with an estimated incidence of 1.2-2.3 per 100,000 population per year [3]. Miller Fisher syndrome (MFS) is a rare variant of GBS, with an annual incidence of 0.09 per 100,000 [4]. In contrast to the generalised limb weakness and sensory symptoms often seen in GBS, the clinical manifestations of MFS are restricted to ophthalmoplegia, limb ataxia, and loss of deep tendon reflexes [3, 5-7]. In addition to MFS, there are other variants and subtypes of GBS, such as acute motor (and sensory) axonal neuropathy, acute inflammatory demyelinating polyneuropathy, acute panautonomic neuropathy, and Bickerstaff brainstem encephalitis. Increasingly these syndromes are understood as representing discrete parts of a continuous spectrum of disease characterised by immune-complex mediated demyelination at sites throughout the nervous system [3, 8, 9]. Accordingly there is significant overlap between these syndromes with patients presenting with features of both GBS and MFS.
GBS typically presents with a rapidly progressing (over several days) weakness, often associated with pain, sensory impairment, and paraesthesiae affecting the limbs in a relatively symmetrical pattern. Involvement of respiratory muscles can lead to respiratory failure and death. Careful monitoring of vital capacity is therefore required to detect the 25% of severely affected patients who will need artificial ventilation [3].
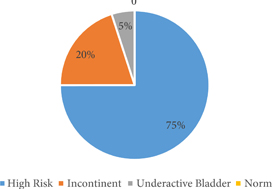
Unusual patterns of muscle involvement can occur. There are several reports in the literature of patients presenting with AUR as the initial symptom of GBS [10-16]. Urinary dysfunction occurs in approximately 25% of patients with GBS, with AUR in 10% [13, 14, 17]. This is thought to be due to a combination of hypo- and hyper-activity in both the parasympathetic and sympathetic innervation of the bladder and urethra [12-14]. The prevalence of bladder dysfunction in MFS is unknown [17]. Approximately two-thirds of GBS patients have symptoms of autonomic dysfunction. Symptoms include cardiac arrhythmias, paralytic ileus, sustained hypertension, and sudden asystole [3, 11, 18, 19].
The underlying pathology in GBS (and variants) is thought to be an immune-complex mediated damage to peripheral nerves. Antibodies to various gangliosides (e.g., GM1, GM1b, GD1a, GalNAc-GD1a, GD3, GT1a, and GQ1b) on the surface of neurons have been found in the serum of patients with GBS [3]. These bind to the cell-surface antigen, activate the complement cascade, and thereby damage the myelin sheath, the axolemma, or voltage-gated cation channels. The resulting impaired nerve conduction leads to the observed clinical features. Because of differential expression of gangliosides across neuronal types, different patterns of antibody production are associated with distinct syndromes. Acute motor (and sensory) axonal neuropathy is associated with anti-GM1, -GM1b, -GD1a, and -GalNAc-GD1a antibodies, whereas MFS and GBS with ophthalmoplegia is associated with anti-GD3, -GT1a, and -GQ1b antibodies [3, 7, 20].
Approximately 85% of patients with MFS have detectable anti-GQ1b antibodies during the first week of the illness [21]. The high sensitivity and specificity of this serological finding for MFS makes it a useful diagnostic test. The classical CSF finding in GBS (and variants) is an acellular sample with an elevated protein concentration. In MFS only 25% of patients have an elevated CSF protein level during the first week, increasing to 85% by the third week. This is in contrast to GBS, where 45% have an elevated protein in week one, and 75% by week three [21]. Our patient exhibited neither elevated CSF protein concentration, nor anti-GQ1b antibodies. This may be related to the timing of the tests.
In support of the diagnosis of a post-infectious neuropathy, our patient experienced a febrile illness characterised by gastrointestinal disturbance several days before the onset of his neurological symptoms. Approximately two-thirds of GBS patients have a history of an antecedent infective illness. The most commonly implicated organism is Campylobacter jejuni [22]. Antibodies are generated to lipooligosaccharides in the cell wall of C. jejuni. These lipooligosaccharides mimic the carbohydrates of gangliosides. Therefore the antibodies cross react with gangliosides on the surface of peripheral neurons causing neurological disturbance. The specific gene variants expressed by the causative microorganism are thought to result in specific patterns of antibody production which lead to the distinct clinical syndromes by virtue of the pattern of expression of the target epitopes [3].
The GQ1b ganglioside is expressed by human oculomotor, abducens, and trochlear nerve fibres but not by other cranial nerves [23]. Oculomotor muscle fibres also express large amounts of GQ1b on their surface [24]. These two targets for anti-GQ1b antibodies (nerve and muscle) are thought to result in the ophthalmoplegia characteristic of MFS.
Regarding autonomic dysfunction, a recent in vitro study has shown that antibodies from GBS patients increase the release of noradrenaline from sympathetic neurons [25]. One previously documented case of AUR in a woman with GBS showed that the retention was due to a non-relaxing internal sphincter, presumably secondary to overactivity of the sympathetic innervation [14]. In a case series, the same authors concluded that the urodynamic abnormalities found in GBS patients were a combination of overactive and underactive detrusor muscle, and an overactive internal sphincter [13]. Wosnitzer et al. [15] reported the case of a 20-year old woman with persistent urinary retention 18 months after the onset of GBS. She was successfully treated with an implantable sacral neuromodulator.
Treatment for GBS involves frequent observation to detect autonomic dysfunction, monitoring of vital capacity, and swallowing, as well as meticulous attention to venous thrombo-embolism prophylaxis in immobilised patients. Immunotherapy with intravenous immunoglobulin or plasma exchange has been shown to significantly improve overall outcome in terms of morbidity and mortality [26]. There are no randomised-controlled trials of immunotherapy for MFS. Typically MFS patients have a good natural recovery, with between 60% and 100% having complete clinical recovery within six months. Immunotherapy is therefore not currently recommended for MFS due to a lack of evidence to support its use [27].
Conclusions
A young patient in acute urinary retention was found to have associated neurological features consistent with a clinical diagnosis of an inflammatory demyelinating polyneuropathy. This was likely Miller Fisher syndrome, although diagnostic testing was inconclusive. This is a rare but important differential diagnosis to consider in patients with bladder dysfunction of neurologic origin, not least because patients with autonomic involvement in an acute peripheral neuropathy may rapidly become unstable, requiring cardio-respiratory support.
References
[1] Selius BA, Subedi R. Urinary retention in adults: diagnosis and initial management. Am Fam Physician. 2008 Mar 1: 77:643-50
[2] Fowler CJ, O’Malley KJ. Investigation and management of neurogenic bladder dysfunction. J Neurol Neurosurg Psychiatry. 2003 Dec: 74 Suppl 4:iv27-iv31
[3] van Doorn PA, Ruts L, Jacobs BC. Clinical features, pathogenesis, and treatment of Guillain-Barre syndrome. Lancet Neurol. 2008 Oct: 7:939-50
[4] Casmiro M, Guarino M, D’Alessandro R. Guillain-Barre syndrome variants in Emilia-Romagna, Italy, 1992-3: incidence, clinical features, and prognosis. Emilia-Romagna Study Group on Clinical and Epidemiological Problems in Neurology. J Neurol Neurosurg Psychiatry. 1998 Aug: 65:218-24
[5] Fisher M. An unusual variant of acute idiopathic polyneuritis: syndrome of ophthalmoplegia, ataxia and areflexia. N Engl J Med. 1956: 255:57-65
[6] Willison HJ, O’Hanlon GM. The immunopathogenesis of Miller Fisher syndrome. J Neuroimmunol. 1999 Dec: 100:3-12
[7] Willison HJ. The immunobiology of Guillain-Barre syndromes. J Peripher Nerv Syst. 2005 Jun: 10:94-112
[8] Nagashima T, Koga M, Odaka M, Hirata K, Yuki N. Continuous spectrum of pharyngeal-cervical-brachial variant of Guillain-Barre syndrome. Arch Neurol. 2007 Oct: 64:1519-23
[9] Yuki N. Fisher syndrome and Bickerstaff brainstem encephalitis (Fisher-Bickerstaff syndrome). J Neuroimmunol. 2009 Oct 30: 215:1-9
[10] Kogan BA, Solomon MH, Diokno AC. Urinary retention secondary to Landry-Guillain-Barre syndrome. J Urol. 1981 Nov: 126:643-4
[11] Labovitz AE, Mangurten HH. Guillain-Barre syndrome presenting with urinary retention and hypertension. Clin Pediatr (Phila). 2004 Sep: 43:659-61
[12] Sakakibara R, Hattori T, Kuwabara S, Yamanishi T, Yasuda K. Micturitional disturbance in patients with Guillain-Barre syndrome. J Neurol Neurosurg Psychiatry. 1997 Nov: 63:649-53
[13] Sakakibara R, Uchiyama T, Kuwabara S, et al. Prevalence and mechanism of bladder dysfunction in Guillain-Barre Syndrome. Neurourol Urodyn. 2009: 28:432-7
[14] Sakakibara R, Uchiyama T, Tamura N, Kuwabara S, Asahina M, Hattori T. Urinary retention and sympathetic sphincter obstruction in axonal Guillain-Barre syndrome. Muscle Nerve. 2007 Jan: 35:111-5
[15] Wosnitzer MS, Walsh R, Rutman MP. The use of sacral neuromodulation for the treatment of non-obstructive urinary retention secondary to Guillain-Barre syndrome. Int Urogynecol J Pelvic Floor Dysfunct. 2009 Sep: 20:1145-7
[16] Wu SH, Lynn JJ, Chan YL, Chiu TF, Chen JC, Chang YC. Acute urinary retention as the initial manifestation of Guillain-Barre syndrome. Am J Emerg Med. 2011 Aug 2:
[17] Kuwabara S. Guillain-Barre syndrome: epidemiology, pathophysiology and management. Drugs. 2004: 64:597-610
[18] Nowe T, Huttemann K, Engelhorn T, Schellinger PD, Kohrmann M. Paralytic ileus as a presenting symptom of Guillain-Barre syndrome. J Neurol. 2008 May: 255:756-7
[19] Patel MB, Goyal SK, Punnam SR, Pandya K, Khetarpal V, Thakur RK. Guillain-Barre Syndrome with asystole requiring permanent pacemaker: a case report. J Med Case Reports. 2009: 3:5
[20] Chiba A, Kusunoki S, Shimizu T, Kanazawa I. Serum IgG antibody to ganglioside GQ1b is a possible marker of Miller Fisher syndrome. Ann Neurol. 1992 Jun: 31:677-9
[21] Nishimoto Y, Odaka M, Hirata K, Yuki N. Usefulness of anti-GQ1b IgG antibody testing in Fisher syndrome compared with cerebrospinal fluid examination. J Neuroimmunol. 2004 Mar: 148:200-5
[22] Hadden RD, Karch H, Hartung HP, et al. Preceding infections, immune factors, and outcome in Guillain-Barre syndrome. Neurology. 2001 Mar 27: 56:758-65
[23] Chiba A, Kusunoki S, Obata H, Machinami R, Kanazawa I. Ganglioside composition of the human cranial nerves, with special reference to pathophysiology of Miller Fisher syndrome. Brain Res. 1997 Jan 16: 745:32-6
[24] Liu JX, Willison HJ, Pedrosa-Domellof F. Immunolocalization of GQ1b and related gangliosides in human extraocular neuromuscular junctions and muscle spindles. Invest Ophthalmol Vis Sci. 2009 Jul: 50:3226-32
[25] Lehmann HC, Jangouk P, Kierysch EK, Meyer zu Horste G, Hartung HP, Kieseier BC. Autoantibody-mediated dysfunction of sympathetic neurons in Guillain-Barre syndrome. Arch Neurol. 2010 Feb: 67:203-10
[26] Hughes RA, Swan AV, Raphael JC, Annane D, van Koningsveld R, van Doorn PA. Immunotherapy for Guillain-Barre syndrome: a systematic review. Brain. 2007 Sep: 130:2245-57
[27] Overell JR, Hsieh ST, Odaka M, Yuki N, Willison HJ. Treatment for Fisher syndrome, Bickerstaff’s brainstem encephalitis and related disorders. Cochrane Database Syst Rev. 2007:CD004761