BAUS – BJUI – USANZ Joint Session at AUA 2024
Urological Management has Impact
Saturday, May 4th 1:00 – 4.00 PM
Room 207, Henry B. González Convention Center
Saturday, May 4th 1:00 – 4.00 PM
Room 207, Henry B. González Convention Center
In the week following Britain’s exit from Europe after the BREXIT referendum, BAUS 2016 got underway in Liverpool’s BT convention Centre. This was the 72nd meeting of the British Association of Urological Surgeons and it was well attended with 1120 delegates (50% Consultant Member Urologists, 30% Trainees, 10% Non member Urologists/Other, 10% Nurses, HCP’S, Scientists).
Monday saw a cautionary session on medicolegal aspects in Andrology, focusing on lawsuits over the last year. Mr Mark Speakman presented on the management issue of testicular torsion. This sparked further discussion on emergency cover for paediatrics with particular uncertainty noted at 4 and 5 year olds and great variation in approach dependent on local trust policy. Mr Julian Shah noted the most litigious areas of andrology, with focus on cosmesis following circumcisions. Therefore serving a reminder on the importance of good consent to manage patients’ expectations.
In the Dragons’ Den, like the TV show, junior urologists pitched their ideas for collaborative research projects, to an expert panel. This year’s panel was made up of – Mark Emberton, Ian Pearce, and Graeme MacLennan. The session was chaired by Veeru Kasivisvanathan, Chair of the BURST Research Collaborative.
Eventual winner Ben Lamb, a trainee from London, presented “Just add water”. The pitch was for an RCT to investigate the efficacy of water irrigation following TURBT against MMC in reducing tumour recurrence. Ben proposed that water, with its experimental tumouricidal properties, might provide a low risk, low cost alternative as an adjuvant agent following TURBT. Judges liked the scientific basis for this study and the initial planning for an RCT. The panel discussed the merits of non-inferiority vs. superiority methodology, and whether the team might compare MMC to MMC with the addition of water, or water instead of MMC. They Dragons’ suggested that an initial focus group to investigate patients’ views on chemotherapy might help to focus the investigation and give credence to the final research question, important when making the next pitch- to a funding body, or ethics committee.
Other proposals were from Ryad Chebbout, working with Marcus Cumberbatch, an academic trainee from Sheffield. Proposing to address the current controversy over the optimal surgical technique for orchidopexy following testicular torsion. His idea involved conducting a systematic review, a national survey of current practice followed by a Delphi consensus meeting to produce evidence based statement of best practice. The final presentation was from Sophia Cashman, East of England Trainee for an RCT to assess the optimal timing for a TWOC after urinary retention. The panel liked the idea of finally nailing down an answer to this age-old question.
Waking up on Tuesday with England out of the European football cup as well as Europe the conference got underway with an update from the PROMIS trial (use of MRI to detect prostate cancer). Early data shows that multi-parametric MRI may be accurate enough to help avoid some prostate biopsies.
The SURG meeting provided useful information for trainees, with advice on progressing through training and Consultant interviews. A debate was held over run through training, which may well be returning in the future. The Silver cystoscope was awarded to Professor Rob Pickard voted for by the trainees in his deanery, for his devotion to their training.
Wednesday continued the debate on medical expulsion therapy (MET) for ureteric stones following the SUSPEND trial. Most UK Urologists seem to follow the results of the trial and have stopped prescribing alpha blockers to try and aid stone passage and symptoms. However the AUA are yet to adopt this stance and feel that a sub analysis shows some benefit for stones >5mm, although this is not significant and pragmatic outcomes. Assistant Professor John Hollingsworth (USA) argued for MET, with Professor Sam McClinton (UK) against. A live poll at the end of the session showed 62.9% of the audience persuaded to follow the SUSPEND trial evidence and stop prescribing MET.
In the debate of digital versus fibreoptic scopes for flexible ureteroscopy digital triumphed, but with a narrow margin.
In other updates and breaking news it appears that BCG is back! However during the shortage EMDA has shown itself to be a promising alternative in the treatment of high grade superficial bladder cancer.
The latest BAUS nephrectomy data shows that 90% are performed by consultant, with 16 on average per consultant per year. This raises some issues for registrar training, however with BAUS guidelines likely to suggest 20 as indicative numbers this is looking to be an achievable target for most consultants. Robotic advocates will be encouraged, as robotic partial nephrectomy numbers have overtaken open this year. The data shows 36% of kidney tumours in the under 40 years old are benign. Will we have to consider biopsying more often? However data suggests we should be offering more cytoreductive nephrectomies, with only roughly 1/10 in the UK performed compared to 3/10 in the USA.
The andrology section called for more recruitment to The MASTER trial (Male slings vs artificial urinary sphincters), whereas the OPEN trial has recruited(open urethroplasty vs optical urethotomy). In the treatment of Peyronie’s disease collagenase has been approved by NICE but not yet within the NHS.
Endoluminal endourology presentation showed big increases in operative numbers with ureteroscopy up by 50% and flexible ureteroscopy up by 100%. Stents on strings were advocated to avoid troubling stent symptoms experienced by most patients. New evidence may help provide a consensus on defining “stone free” post operation. Any residual stones post-operatively less than 2mm were shown to pass spontaneously and therefore perhaps may be classed as “stone free”.
Big changes seem likely in the treatment of benign prostatic hyperplasia, with a race to replace the old favorite TURP. Trials have of TURP (mono and bipolar) vs greenlight laser are already showing similar 2 year outcomes with the added benefit of shorter hospital stays and less blood loss. UROLIFT is an ever more popular alternative with data showing superiority to TURP in lifestyle measures, likely because it preserves sexual function, and we are told it can be performed as a 15 minute day case operation. The latest new therapy is apparently “Aquabeam Aquablation”, using high pressured water to remove the prostate. Non surgical treatments are also advancing with ever more accurate super selective embolisation of the prostatic blood supply.
This year all accepted abstracts were presented in moderated EPoster sessions. The format was extremely successful removing the need for paper at future conferences? A total of 538 abstracts were submitted and 168 EPosters displayed. The winner of best EPoster was P5-5 Altaf Mangera: Bladder Cancer in the Neuropathic Bladder.
The best Academic Paper winner was Mark Salji of the CRUK Beatson institute, titled “A Urinary Peptide Biomarker Panel to Identify Significant Prostate Cancer”. Using capillary electrophoresis coupled to mass spectrometry (CE-MS) they analysed 313 urine samples from significant prostate cancer patients (Gleason 8-10 or T3/4 disease) and low grade control disease. They identified 94 peptide urine biomarkers which may provide a useful adjunct in identifying significant prostate cancer from insignificant disease.
The Office of Education offered 20 courses. Popular off-site courses were ultrasound for the Urologist, at Broadgreen Hospital, a slightly painful 30 min drive from the conference centre. However well worth the trip, delivered by Radiology consultants this included the chance to scan patients volunteers under guidance, with separate stations for kidneys, bladder and testicles and learning the “knobology” of the machines.
Organised by Tamsin Greenwell with other consultant experts in female, andrology and retroperitoneal cancer, a human cadaveric anatomy course was held at Liverpool university. The anatomy teaching was delivered by both Urology consultants and anatomists allowing for an excellent combination of theory and functional anatomy.
BAUS social events are renowned and with multiple events planned most evenings were pretty lively. The official drinks reception was held at the beautiful Royal Liver Building. The venue was stunning with great views over the waterfront and the sun finally shining. Several awards were presented including the Gold cystoscope to Mr John McGrath for significant contribution to Urology within 10 years appointment as consultant. The Keith Yeates medal was awarded to Mr Raj Pal, the most outstanding candidate in the first sitting of the intercollegiate specilaity examination, with a score of over 80%.
During the conference other BAUS awards presented include the St Peter’s medal was awarded to Margeret Knowles, Head of section of molecular oncology, Leeds Institute of Cancer and Pathology, St James University hospital Leeds. The St Paul’s medal awarded to Professor Joseph A. Smith, Vanderbilt University, Nashville, USA. The Gold medal went to Mr. Tim Terry, Leicester General Hospital.
An excellent industry exhibition was on display, with 75 Exhibiting Companies present. My personal fun highlight was a flexible cystoscope with integrated stent remover, which sparked Top Gear style competiveness when the manufacturer set up a time-trial leaderboard. Obviously this best demonstrated the speed of stent removal with some interesting results…
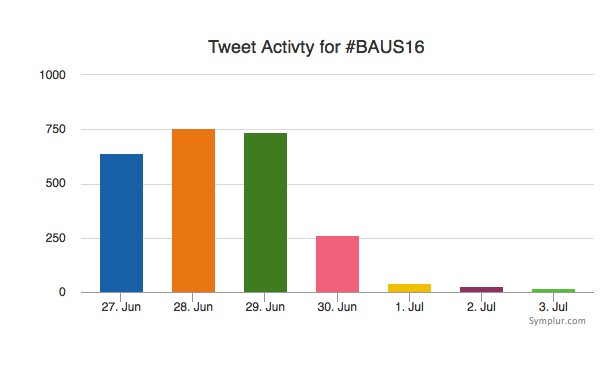
Social media review shows good contribution daily.
Thanks BAUS a great conference, very well organised and delivered with a great educational and social content, looking forward to Glasgow 2017! #BAUS2017 #Glasgow #BAUSurology
Nishant Bedi
Specialist Training Registrar North West London
Twitter: @nishbedi
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Franklin Kuehhas, discussing his paper.
If you only have time to read one article this week, it should be this one.
To present the feasibility and safety of penile length and girth restoration based on a modified ‘sliding’ technique for patients with severe erectile dysfunction (ED) and significant penile shortening, with or without Peyronie’s disease (PD).
Between January 2013 and January 2014, 143 patients underwent our modified ‘sliding’ technique for penile length and girth restoration and concomitant penile prosthesis implantation. It is based on three key elements: (i) the sliding manoeuvre for penile length restoration; (ii) potential complementary longitudinal ventral and/or dorsal tunical incisions for girth restoration; and (iii) closure of the newly created rectangular bow-shaped tunical defects with Buck’s fascia only.
In all, 143 patients underwent the procedure. The causes of penile shortening and narrowing were: PD in 53.8%; severe ED with unsuccessful intracavernosal injection therapy in 21%; post-radical prostatectomy 14.7%; androgen-deprivation therapy, with or without brachytherapy or external radiotherapy, for prostate cancer in 7%; post-penile fracture in 2.1%; post-redo-hypospadias repair in 0.7%; and post-priapism in 0.7%. In patients with ED and PD, the mean (range) deviation of the penile axis was 45 (0‒100)°. The mean (range) subjective penile shortening reported by patients was 3.4 (1‒7) cm and shaft constriction was present in 53.8%. Malleable penile prostheses were used in 133 patients and inflatable penile prostheses were inserted in 10 patients. The median (range) follow-up was 9.7 (6‒18) months. The mean (range) penile length gain was 3.1 (2‒7) cm. No penile prosthesis infection caused device explantation. The average International Index of Erectile Function (IIEF) score increased from 24 points at baseline to 60 points at the 6-month follow-up.
Penile length and girth restoration based on our modified sliding technique is a safe and effective procedure. The elimination of grafting saves operative time and, consequently, decreases the infection risk and costs associated with surgery.
The old goal of prosthetic surgery, which aimed to guarantee a hard and straight penis good enough for penetrative intercourse, is likely to have now become obsolete. Various authors have reported that patients with Peyronie’s disease (PD) and severe corporal fibrosis who undergo penile prosthesis implantation tend to report the lowest satisfaction rates, mainly because of significant penile length loss [1, 2]. In particular, according to Kueronya et al. [3], ~80% of patients affected by PD perceive a degree of penile shortening before surgery, and any further loss of length attributable to the surgical correction leads to bother among all the affected patients. All attempts at penile length restoration during prosthetic surgery should therefore be welcomed in order to achieve higher patient satisfaction.
Initial attempts at penile length restoration involved a full disassembly of the penis and the use of a circumferential graft [4]. Then, in 2012, Rolle et al. [5] described the sliding technique, a modification of the circumferential graft that consists of a double dorsal-ventral patch and should therefore provide more stability to the corpora cavernosa than a circumferential graft.
The present series by Egydio et al. [6] describes a modified sliding technique without grafting the defect of the tunica albuginea. This reduces the operating time and theoretically infection rates should therefore be reduced.
Although leaving a defect in the tunica albuginea should, in theory, lead to a haematoma formation and potentially infection of the device, in the present series, no penile prosthesis infections were reported.
Although we believe that cutting corners in surgery is not the way forward, the authors of the present paper should be congratulated because the postoperative results in their series are very encouraging. In fact, the mean penile length gain in their series was 3.1 cm, with no reported infections requiring the explantation of the penile prosthesis and with an average increase in International Index of Erectile Function score of 36.
Certainly, if the results of the present series can be confirmed in the future, this technique will revolutionize the concept that any tunical defect >1 cm in size needs to be grafted to prevent aneurysmal dilatation of the cylinders of an inflatable penile prosthesis [7], as none of the inflatable cylinders in the series developed aneurysms.
To present the feasibility and safety of penile length and girth restoration based on a modified ‘sliding’ technique for patients with severe erectile dysfunction (ED) and significant penile shortening, with or without Peyronie’s disease (PD).
Between January 2013 and January 2014, 143 patients underwent our modified ‘sliding’ technique for penile length and girth restoration and concomitant penile prosthesis implantation. It is based on three key elements: (i) the sliding manoeuvre for penile length restoration; (ii) potential complementary longitudinal ventral and/or dorsal tunical incisions for girth restoration; and (iii) closure of the newly created rectangular bow-shaped tunical defects with Buck’s fascia only.
In all, 143 patients underwent the procedure. The causes of penile shortening and narrowing were: PD in 53.8%; severe ED with unsuccessful intracavernosal injection therapy in 21%; post-radical prostatectomy 14.7%; androgen-deprivation therapy, with or without brachytherapy or external radiotherapy, for prostate cancer in 7%; post-penile fracture in 2.1%; post-redo-hypospadias repair in 0.7%; and post-priapism in 0.7%. In patients with ED and PD, the mean (range) deviation of the penile axis was 45 (0‒100)°. The mean (range) subjective penile shortening reported by patients was 3.4 (1‒7) cm and shaft constriction was present in 53.8%. Malleable penile prostheses were used in 133 patients and inflatable penile prostheses were inserted in 10 patients. The median (range) follow-up was 9.7 (6‒18) months. The mean (range) penile length gain was 3.1 (2‒7) cm. No penile prosthesis infection caused device explantation. The average International Index of Erectile Function (IIEF) score increased from 24 points at baseline to 60 points at the 6-month follow-up.
Penile length and girth restoration based on our modified sliding technique is a safe and effective procedure. The elimination of grafting saves operative time and, consequently, decreases the infection risk and costs associated with surgery.
Every Month the Editor-in-Chief selects an Article of the Month from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
To examine the efficacy of intralesional collagenase Clostridium histolyticum (CCH) in defined subgroups of patients with Peyronie’s disease (PD).
The efficacy of CCH compared with placebo, assessed from baseline to week 52, was examined in subgroups of participants from the Investigation for Maximal Peyronie’s Reduction Efficacy and Safety Studies (IMPRESS) I and II. The subgroups were defined according to: severity of penile curvature deformity at baseline (30–60° [n = 492] and 61–90° [n = 120]); PD duration (1 to ≤2 [n = 201], >2 to ≤4 [n = 212] and >4 years [n = 199]); degree of plaque calcification (no calcification [n = 447], non-contiguous stippling [n = 103] and contiguous calcification that did not interfere with injection of CCH [n = 62]); and baseline erectile function (International Index of Erectile Function [IIEF] scores 1–5 [n= 22], 6–16 [n = 106] and ≥17 [n = 480]).
Reductions in penile curvature deformity and PD symptom bother were observed in all subgroups. Penile curvature deformity reductions were significantly greater with CCH than with placebo for the following subgroups: baseline penile curvature 30–60° and 61–90°; disease duration >2 to ≤4 years and >4 years; no calcification; and IIEF score ≥17 (high IIEF-erectile function score; P < 0.05 for all). PD symptom bother reductions were significantly greater in the CCH group for: penile curvature 30–60°; disease duration >4 years; no calcification; and IIEF score 1–5 (no sexual activity) and ≥17 (P < 0.05 for all).
In this analysis, clinical efficacy of CCH treatment for reducing penile curvature deformity and PD symptom bother was found across subgroups. In the IMPRESS I and II overall, adverse events (AEs) were typically mild or moderate, although treatment-related serious AEs, including corporal rupture or penile haematoma, occurred. Future studies could be considered to directly assess the efficacy and safety of CCH treatment in defined subgroups of PD patients, with the goal of identifying predictors of optimum treatment success.
The study by Lipshultz et al. [1] is a post hoc reworking of the results of the Investigation for Maximal Peyronie’s Reduction Efficacy and Safety Studies (IMPRESS) I and II phase 3 trials (each included 418 randomised patients) of intralesional injections of collagenase clostridium histolyticum (CCH) in patients with Peyronie’s disease (PD). The intention being to identify specifically, which subgroups of patients with PD might do best with CCH treatment compared with their matched placebo controls, as determined by reductions in penile curvature deformity and Peyronie’s Disease Questionnaire (PDQ) PD Symptom Bother score at study week 52 compared with baseline.
In both IMPRESS studies, CCH-treated patients showed statistically greater mean improvements vs placebo for reduction of penile curvature and PDQ PD Symptom Bother score. The current authors [1] have reassessed these previous results using four patient cohort variables, namely, baseline penile curvature, duration of PD, degree of penile calcification, and baseline erectile function severity, which were then further divided using various descriptors.
The results show that intralesional CCH significantly reduced baseline penile curvature in both the 30–60 and 61–90° curvature cohorts (P < 0.001 and P <0.008, respectively). Additionally, significant penile curvature improvements occurred with intralesional CCH when PD duration was >2 to <4 years and >4 years (P < 0.001).
CCH treatment in patients with PD with no penile calcification show statistically significant improvements in reducing baseline penile curvature and PDQ PD Symptom Bother score but this was not seen for either the noncontiguous stippling or contiguous calcification patient subgroups. Significant improvements in penile curvature occurred with intralesional CCH in patients with PD with a baseline International Index of Erectile Function (IIEF) score of >17 (P < 0.001) and the PDQ PD Symptom Bother score was also significantly reduced in these patients. Although these results are statistically meaningful, the clinical benefits are less readily discernible considering 12.5° was the largest difference in the reduction of mean penile curvature in all subgroups when comparing intralesional CCH to placebo at week 52. Similarly, although statistically significant changes in the PDQ PD Symptom Bother score were reported for intralesional CCH for the subgroups with duration of disease of >4 years, no penile calcification, and IIEF of >17, it is unclear what clinical benefit would accrue with a maximal change of 1.4 in any of the randomised subgroups.
Importantly, the IMPRESS I and II studies were not designed for subgroup analysis and despite combining these studies some of the specified PD subgroups contained in the present paper contain too few subjects to allow a valid statistical analysis of CCH efficacy. This has prompted the authors to conclude that further adequately powered prospective, randomised studies should be conducted to further clarify which PD characteristics offer optimal patient benefit with CCH treatment. The outcomes of these future studies might then optimise healthcare expenditure for a non-surgical treatment (consisting of eight penile injections and modelling), which shows therapeutic promise for patients with PD but potentially has significant consumer cost issues, which may be prohibitive unless some clinician guidelines exist for the use of CCH treatment. This has relevance as the USA Food and Drug Administration has already approved the use of intralesional CCH for the treatment of adult men with PD, who at the start of therapy have a palpable plaque and a curvature deformity of ≥30° [2].
Importantly, the outcomes of the patients with PD in the IMPRESS studies were only reported to week 52 of the study, which begs the questions as to how long any clinical benefit might last in patients who initially respond to intralesional CCH and whether these patients once having relapsed might respond to adjuvant injections.
Every Week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Franklin Emmanuel Kuehhas, discussing his paper.
If you only have time to read one article this week, it should be this one.
To compare patient-reported outcomes (PROs) of surgical correction of Peyronie’s disease (PD) with the Nesbit procedure, plaque incision and grafting, and the insertion of a malleable penile implant after surgical correction of penile curvature.
We performed a retrospective review of men who underwent surgical correction of PD between January 2010 and December 2012 at six international centres. Treatment-related PROs and satisfaction were evaluated with a non-validated questionnaire.
The response rate to the questionnaire was 70.9%, resulting in a study cohort of 206 patients. The Nesbit procedure, plaque incision with grafting, or implantation of a malleable penile prosthesis was performed in 50, 48, and 108 patients, respectively. Overall, 79.1% reported a subjective loss of penile length due to PD preoperatively (range 2.1–3.2 cm). Those patients treated with a malleable penile implant reported the greatest subjective penile length loss, due to PD. A subjective loss of penile length of >2.5 cm resulted in reduced preoperative sex ability. Postoperatively, 78.0%, 29.2% and 24.1% patients in the Nesbit, grafting, and implant groups reported a postoperative, subjective loss of penile length (range 0.4–1.2 cm), with 86.3%, 78.6%, and 82.1% of the patients in each group, respectively, being bothered by the loss of length.
Penile length loss due to PD affects most patients. Further penile length loss due to the surgical correction leads to bother among the affected patients, irrespective of the magnitude of the loss. The Nesbit procedure was associated with the highest losses in penile length. In patients with PD and severe erectile dysfunction, a concomitant lengthening procedure may be offered to patients to help overcome the psychological burden caused by the loss of penile length.
Peyronie’s disease (PD) is an acquired benign connective tissue disorder of the tunica albuginea of the penis that leads to the formation of fibrous inelastic plaques. As a result of pain, worsening quality of erections, penile shortening and deformity, the quality of life of both the patient and their partner may be significantly affected, and this may lead to depression, low self-esteem and relationship difficulties [1].
At present, surgery represents the ‘gold standard’ treatment when PD is stable, and should be offered to guarantee a penis straight and rigid enough to allow penetrative intercourse.
The flow chart in the 2010 guidelines on PD indicates the type of surgery that should be offered according to the preoperative quality of the erection, degree of deformity and penile length, but patient perception of preoperative penile shortening is not taken into consideration [2]. Penile shortening does play an important part, however, with regard to postoperative patient satisfaction, as confirmed by Akin-Olugbade et al. [3], whose series of patients with PD reported the lowest satisfaction rates after penile prosthesis implantation.
According to the present series by Kueronya et al. [4], in which patient-perceived pre- and postoperative penile length loss in patients with PD was evaluated, 79.1% of patients perceived a degree of length loss attributable to PD, and a subjective loss of length of >2.5 cm translated into reduced ability with regard to sexual intercourse. In particular, patients who underwent penile prosthesis implantation reported more significant perceived shortening. This is not surprising, as patients with larger plaques, more severe forms of PD and fibrosis are more likely to have erectile dysfunction and ultimately to require a penile prosthesis implantation. Among patients who did not undergo penile prosthesis implantation, those requiring Nesbit plication reported less preoperative shortening than those requiring plaque incision and grafting, as the latter group presented with more severe deformities.
Further penile length loss caused by the surgical correction leads to bother to the patients, irrespective of the magnitude of the loss. The message from the present series by Kueronya et al. is that, to achieve higher postoperative satisfaction rates in this unfortunate cohort of patients, the choice of the type of surgery should take into consideration patient’s perceived preoperative penile shortening and not be based solely on the 2010 PD guidelines algorithm, because ultimately patients wish to obtain full restoration of the shape and size of penis they had before the onset of PD [2].
As patient’s perceived penile length plays such an important role in a patient’s postoperative satisfaction and because patients undergoing penile prosthesis implantation are those who have lost more length, length restoration should be offered simultaneously with penile prosthesis implantation [5, 6].
Kueronya et al. should be congratulated for their work, which is the first series evaluating patient’s perceived penile shortening and may represent a significant step towards the restoration of an adequate sex life in patients with PD.
To compare patient-reported outcomes (PROs) of surgical correction of Peyronie’s disease (PD) with the Nesbit procedure, plaque incision and grafting, and the insertion of a malleable penile implant after surgical correction of penile curvature.
We performed a retrospective review of men who underwent surgical correction of PD between January 2010 and December 2012 at six international centres. Treatment-related PROs and satisfaction were evaluated with a non-validated questionnaire.
The response rate to the questionnaire was 70.9%, resulting in a study cohort of 206 patients. The Nesbit procedure, plaque incision with grafting, or implantation of a malleable penile prosthesis was performed in 50, 48, and 108 patients, respectively. Overall, 79.1% reported a subjective loss of penile length due to PD preoperatively (range 2.1–3.2 cm). Those patients treated with a malleable penile implant reported the greatest subjective penile length loss, due to PD. A subjective loss of penile length of >2.5 cm resulted in reduced preoperative sex ability. Postoperatively, 78.0%, 29.2% and 24.1% patients in the Nesbit, grafting, and implant groups reported a postoperative, subjective loss of penile length (range 0.4–1.2 cm), with 86.3%, 78.6%, and 82.1% of the patients in each group, respectively, being bothered by the loss of length.
Penile length loss due to PD affects most patients. Further penile length loss due to the surgical correction leads to bother among the affected patients, irrespective of the magnitude of the loss. The Nesbit procedure was associated with the highest losses in penile length. In patients with PD and severe erectile dysfunction, a concomitant lengthening procedure may be offered to patients to help overcome the psychological burden caused by the loss of penile length.