15 years ago, many people reading this blog won’t have even had a mobile phone! Fast forward to today and we wouldn’t leave home without it. Not content with just having a phone, we now crave the multimedia functionality of smartphones which dominate the market. With this ability to spread and share information so easily comes medico-legal dangers, not only for individuals but also hospitals concerned about patient confidentiality for which they are corporately responsible.
Not long ago, taking a picture of a medical condition for any purpose was a major effort. Contacting the medical photography department of the hospital would take an age and often the moment would be lost. Things began to change with affordable digital cameras although images were usually stored in one location on that camera, often locked away. This situation has altered completely with mobile phone now offering cameras capable of extremely high quality photography (I don’t own one but the Samsung Galaxy S4 possesses a 16MP lens offering far greater resolution than my digital SLR which is only a few years old and Nokia have just released a 41MP cameraphone!). Here you will get the brief idea about the wired vs wireless security system. Suddenly if we see an interesting condition, we can whip our phones out, take a picture and immediately send it round the world on social media platforms. Even if the photos are just stored on the phone, with these being such desirable objects for thieves, this poses a significant risk to loss of that data and potential breach of patient confidentiality. It used to be that CCTV cameras were all that was required to ensure that things ran well in terms of security within a business. Tough circumstances, on the other hand, necessitate even harder measures, which necessitate the installation of detection and alarm systems. The fact that these commercial access control systems are available in a number of models is the nicest part about them.
So where am I going with this ? Well, I read with interest a recent article on “Clinicians and their Cameras” in Australian Health Review 2013. In this survey of one hospital in Australia, one fifth of clinicians reported using their personal mobile phones for medical photography. The authors describe as “endemic” the non-compliance with policy requirements for written consent for these images. Only 6% disposed of the images according to hospital protocol. What is scary is that I suspect the use of personal mobile phones may be under-reported!
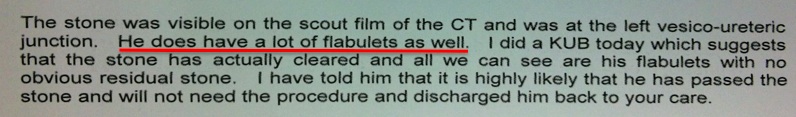
There are many benefits to being able to immediately take a medical image in an appropriately consented patient. It may allow a condition to be tracked e.g. serial photographs of cellulitis; or allow discussion with a senior doctor where the most salient image e.g. the infected wound or an x-ray could even be sent to the consultant at home to review. These moments require spontaneity or the chance is lost.
Many hospitals, certainly in the NHS in the UK, completely ban the use of mobile phones for photography. This is an understandable corporate response to the problem which includes consent, confidentiality, appropriate use, storage and disposal.
Medical staff clearly need to be aware of the ethical issues and regulations regarding the use of medical images. The European Commission has found that collection of medical data and maintenance of medical records fall within the sphere of Article 8 of the European Convention on Human Rights. Thus failure to comply with regulations not only contravenes policy from your employer and regulatory body but also breaches the patients human rights. In the UK the Data Protection Act states that all organisations have a legal obligation to protect personal data which would include an individual taking images on any device and thus non-compliance also breaks the law.
The General Medical Council (GMC) in the UK has guidance on visual and audio recordings of patients. This makes clear the following points:
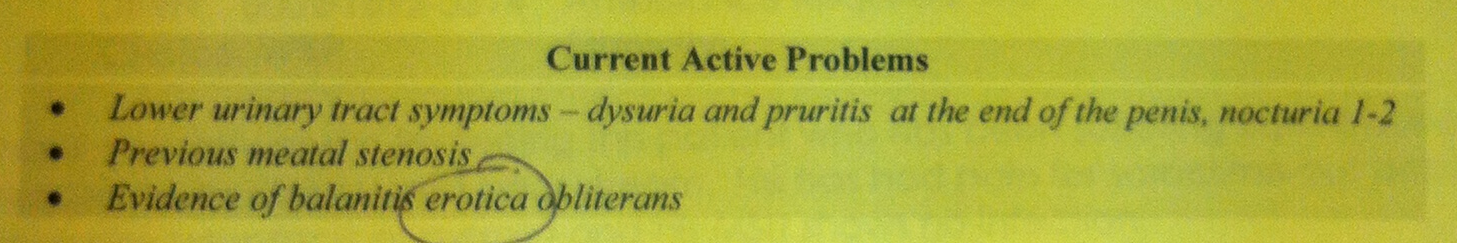
- Appropriate consent must be obtained. This seems obvious although the guidance does say that separate consent is not necessary for images of internal organs, images of pathology slides, endoscopic images, x-ray and ultrasound images. These maybe used for “secondary purposes” without seeking consent if appropriately anonymised and non-recognisable. However this only applies if they are taken as part of the patient’s care. Images for research, teaching or training require appropriate consent which should be stored with the image.
- All images should be anonymised/coded for storage. What mechanisms exist for this in your hospitals?
- Images should be stored securely and follow local procedures and protocols. Fine in principal but how does this work in practice?
- Recordings or images form part of the medical record. So if we do take an image we are responsible for ensuring it is accessible as part of the medical record.
But what about the unexpected finding in the middle of a case? The GMC guidance is clear: In this situation “you must not make recordings for secondary purposes without consent”. So you need it in advance if you are going to do it.
This study suggests that the use of mobile phones for photography in hospitals is commonplace and local protocols are not met. This is likely to be a widespread problem in hospitals in many countries. In my hospital the policy is clear: NO PHOTOGRPAHY ON PHONES OR PERSONAL DEVICES IN THE HOSPITAL. Any breach of this is a disciplinary offence. This prompted the following response from one of my colleagues: “This is ridiculous on many fronts. Bad for patient care, bad for education”. From a managerial perspective I can understand this. From a clinician’s point-of-view, I find this very sad with multiple opportunities lost for improving patient care and medical education. In a highly regulated workplace these rules are likely here to stay and we must all ensure we are compliant with them to avoid potential disciplinary action. I would be interested in the experiences and opinions of readers from other hospitals and countries.
Matthew Bultitude
BJUI Associate Editor