Article of the Week: Does timing matter in postoperative RT for patients at high-risk of recurrence after RP?
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Peter Carroll, discussing his paper.
If you only have time to read one article this week, it should be this one.
Postoperative radiation therapy for patients at high-risk of recurrence after radical prostatectomy: does timing matter?
OBJECTIVE
To evaluate among radical prostatectomy (RP) patients at high-risk of recurrence whether the timing of postoperative radiation therapy (RT) (adjuvant, early salvage with detectable post-RP prostate-specific antigen [PSA], or ‘late’ salvage with a PSA level of >1.0 ng/mL) is significantly associated with overall survival (OS), prostate-cancer specific survival or metastasis-free survival, in a longitudinal cohort.
PATIENTS AND METHODS
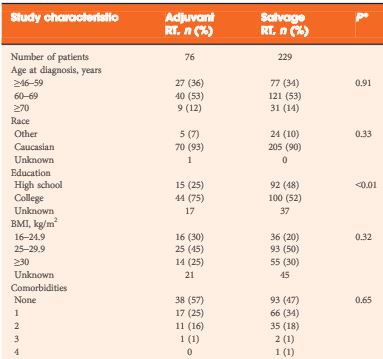
Of 6 176 RP patients in the Cancer of the Prostate Strategic Urologic Research Endeavor (CaPSURE), 305 patients with high-risk pathological features (margin positivity, Gleason score 8–10, or pT3–4) who underwent postoperative RT were examined, either in the adjuvant (≤6 months after RP with undetectable PSA levels, 76 patients) or salvage setting (>6 months after RP or pre-RT PSA level of >0.1 ng/mL, 229 patients). Early (PSA level of ≤1.0 ng/mL, 180 patients) or late salvage RT (PSA level >1.0 ng/mL, 49 patients) was based on post-RP, pre-RT PSA level. Multivariable Cox regression examined associations with all-cause mortality and prostate cancer-specific mortality and/or metastases (PCSMM).
RESULTS
After a median of 74 months after RP, 65 men had died (with 37 events of PCSMM). Adjuvant and salvage RT patients had comparable high-risk features. Compared with adjuvant, salvage RT (early or late) had an increased association with all-cause mortality (hazard ratio [HR] 2.7, P = 0.018) and with PCSMM (HR 4.0, P = 0.015). PCSMM-free survival differed by further stratification of timing, with 10-year estimates of 88%, 84%, and 71% for adjuvant, early salvage, and late salvage RT, respectively (P = 0.026). For PCSMM-free survival and OS, compared with adjuvant RT, late salvage RT had statistically significantly increased risk; however, early salvage RT did not.
CONCLUSION
This analysis suggests that patients who underwent early salvage RT with PSA levels of <1.0 ng/mL may have comparable metastasis-free survival and OS compared with adjuvant RT; however, late salvage RT with a PSA level of >1.0 ng/mL is associated with worse clinical outcomes.