Video: Prostate cancer in kidney transplant recipients – a nationwide register study
:
Prostate cancer in kidney transplant recipients – a nationwide register study
Abstract
Objective
To investigate whether post‐transplantation immunosuppression negatively affects prostate cancer outcomes in male kidney transplant recipients.
Patients and Methods
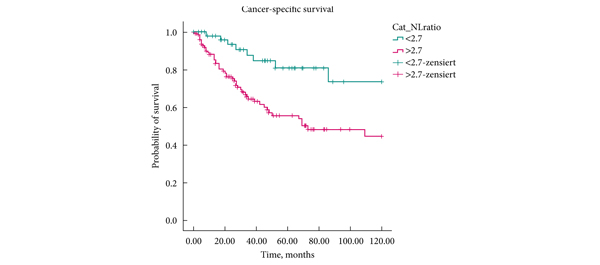
We used the Swedish Renal Register and the National Prostate Cancer Register to identify all kidney transplantation recipients diagnosed with prostate cancer in Sweden 1998–2016. After linking these registers with Prostate Cancer Database Sweden (PCBaSe), a case‐control study was designed to compare time period and risk category‐specific probabilities of a prostate cancer diagnosis amongst kidney transplantation recipients versus the male general population. The registers did not include information about the specific immunosuppression agent used in all transplantation recipients. Data from PCBaSe were used to compare prostate cancer characteristics at diagnosis and survival for patients with prostate cancer with versus without a kidney transplant. Propensity score matching, Cox regression analysis and Fisher’s exact test were used and 95% confidence intervals (CIs) calculated.
Results
Almost half of the 133 kidney transplantation recipients were transplanted before the mid‐1990s, when PSA testing became common. The transplant recipients were not more likely than age‐matched control men to be diagnosed with any (odds ratio [OR] 0.84, 95% CI 0.70–0.99) or high‐risk or metastatic prostate cancer (OR 0.84, 95% CI 0.62–1.13). None of the ORs for the different categories of prostate cancer increased with time since transplantation. Cancer characteristics at the time of diagnosis and cancer‐specific survival were similar amongst transplant recipients and the control group of 665 men diagnosed with prostate cancer without a kidney transplant.
Conclusions
This Swedish nationwide, register‐based study gave no indication that immunosuppression after kidney transplantation increases the risk of prostate cancer or adversely affects prostate cancer outcomes. The study suggests that men with untreated low‐grade prostate cancer can be accepted for transplantation.