Article of the Month: Retzius-sparing RARP using the Revo-i: results of the first human trial
Every Month, the Editor-in-Chief selects an Article of the Month from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
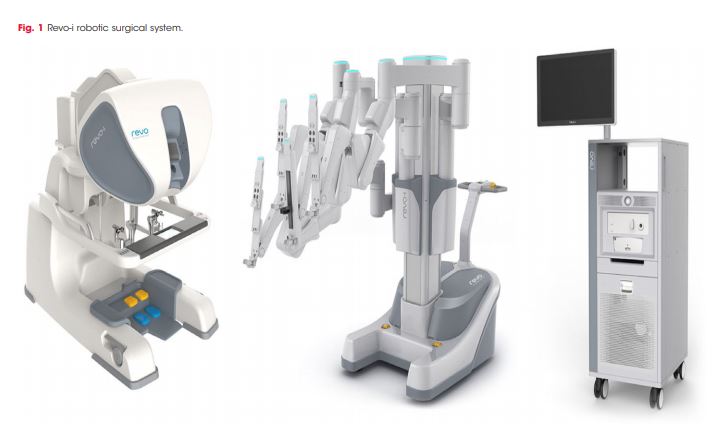
Retzius-sparing robot-assisted radical prostatectomy using the Revo-i robotic surgical system: surgical technique and results of the first human trial
Ki Don Chang*†, Ali Abdel Raheem*‡, Young Deuk Choi* , Byung Ha Chung* and Koon Ho Rha*
*Department of Urological Science Institute, Yonsei University College of Medicine, Seoul, †Department of Urology, Urological Science Institute, Yonsei Wonju University College of Medicine, Wonju, Korea, and ‡Department of Urology, Tanta University Medical School, Tanta, Egypt
Abstract
Objective
To evaluate the safety and proficiency of the Revo‐i® robotic platform (Meere Company Inc.) in the treatment of prostate cancer (PCa).
Patients and Methods
A prospective study was carried out on 17 patients with clinically localized PCa treated between 17 August 2016 and 23 February 2017 at our urology department using the Revo‐i. Patients underwent Retzius‐sparing robot‐assisted radical prostatectomy (RS‐RARP). The primary objective was to describe the RS‐RARP step‐by‐step surgical technique using the Revo‐i. In addition, the safety of the Revo‐i was assessed according to intra‐operative and the postoperative complications within 30 days of surgery. Early oncological outcomes were also assessed according to surgical margin status and biochemical recurrence (BCR). Continence was defined as use of no or only one pad. Surgeons’ satisfaction with the Revo‐i was assessed using the Likert scale.
Results
All surgeries were completed successfully, with no conversion to open or laparoscopic surgery. The median patient age was 72 years. The median docking time, console time, urethrovesical anastomosis time and estimated blood loss were 8 min, 92 min, 26 min and 200 mL, respectively. One patient was transfused intra‐operatively as a result of blood loss of 1 500 mL. Postoperatively, two patients received blood transfusion, and there were no other serious/major complications. The median hospital stay was 4 days. At 3 months, four patients had positive surgical margins, one patient had BCR, and 15 patients were continent. Most of surgeons were satisfied with the Revo‐i performance.
Conclusions
The first human study for the treatment of patients with localized PCa using the Revo‐i robotic surgical system was carried out successfully. The peri‐operative, early oncological and continence outcomes are encouraging. Further prospective studies are warranted to support our preliminary results.