Editorial: Perioperative aspirin: To give or not to give?
As the population ages and life expectancy increases, one may safely assume that more men will be diagnosed with diseases of the elderly such as prostate cancer. In the USA, it is estimated that the number of older adults (≥65 years old) will double between 2010 and 2030, contributing to a 45% increase in cancer incidence [1]. Also, it is likely that these older patients will present with multiple comorbidities, commonly described as ‘multimorbidity’ in the contemporary medical literature, including chronic cardiac and pulmonary conditions requiring multidisciplinary medical management.
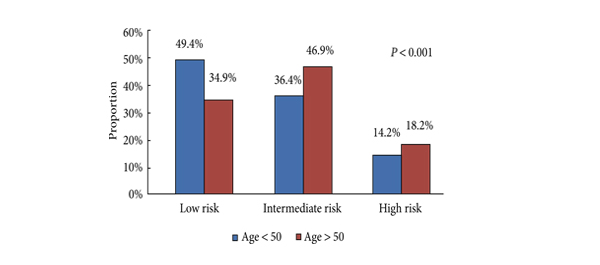
Hence, the present study by Leyh-Bannurah et al. [2] examining the peri-operative use of aspirin in patients undergoing radical prostatectomy (RP) is a timely and important contribution, and may very well influence our clinical decision-making regarding the perioperative management of the anti-coagulated patient. Their results show that perioperative continuation of aspirin made no difference in peri and postoperative outcomes following RP. Previous studies have assessed the effect of aspirin continuation in patients undergoing minimally invasive RP, but the present study is the first to evaluate the effect of aspirin continuation in patients undergoing minimally invasive and open RP at a high-volume tertiary centre. Studies from other surgical specialties evaluating the role of anti-platelet therapy and its timing before surgery have shown conflicting results. The study by Park et al. [3], looking at discontinuation of aspirin for ≥7 days vs <7 days before surgery in patients undergoing lumbar spinal fusion, found that aspirin discontinued only 3–7 days before surgery significantly increased the risk of intraoperative bleeding. Alghamdi et al. [4] found similar results in patients undergoing coronary artery bypass grafting. In contrast, the study by Wolf et al. [5] showed that continuation of aspirin up to the day of the surgery did not increase the risk of bleeding, transfusion or other adverse outcomes in patients undergoing pancreatectomy. Similarly, Khudairy et al. [6] assessed the use of clopidogrel and its discontinuation time in hip fracture repair, and found that whether it was stopped ≥1 week or <1 week before surgery did not make any difference to the risk of bleeding or peri-operative complications. Nonetheless, the evidence provided by the present study by Leyh-Bannurah et al. is important, as the risk of bleeding seems to be procedure-specific, depending on the nature and source of potential bleeding (primarily arterial vs primarily venous). The lack of information, however, regarding cardiovascular morbidities in their patient population is an important limitation of their study; as such factors may influence perioperative decision-making, including the threshold for transfusion.
Akshay Sood and Quoc-Dien Trinh*
VUI Center for Outcomes Research, Analytics and Evaluation, Henry Ford Health System, Detroit, MI, and *Division of Urologic Surgery and Center for Surgery and Public Health, Brigham and Women’s Hospital/Dana-Farber Cancer Institute, Harvard Medical School, Boston, MA, USA
References
- Lamb A. Fast Facts: prostate cancer, seventh edition. BJU Int 2012; 110: E157
-
Leyh-Bannurah S-R, Hansen J, Isbarn H et al. Open and robotic assisted radical retropubic prostatectomy in men with ongoing low-dose aspirin medication: revisiting old paradigm? BJU Int 2014; 114: 396–403
- Park JH, Ahn Y, Choi BS et al. Antithrombotic effects of aspirin on 1- or 2-level lumbar spinal fusion surgery: a comparison between 2 groups discontinuing aspirin use before and after 7 days prior to surgery. Spine 2013; 38: 1561–1565
- Alghamdi AA, Moussa F, Fremes SE. Does the use of preoperative aspirin increase the risk of bleeding in patients undergoing coronary artery bypass grafting surgery? Systematic review and meta-analysis. J Cardiac Surg 2007; 22: 247–256
- Wolf AM, Pucci MJ, Gabale SD et al. Safety of perioperative aspirin therapy in pancreatic operations. Surgery 2014; 155: 39–46
- Al Khudairy A, Al-Hadeedi O, Sayana MK, Galvin R, Quinlan JF. Withholding clopidogrel for 3 to 6 versus 7 days or more before surgery in hip fracture patients. J Orthop Surg 2013; 21: 146–150