Article of the week: Multicentre international experience of 532‐nm laser PVP with GreenLight XPS in men with very large prostates
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
If you only have time to read one article this week, it should be this one.
*Division of Urology, Centre Hospitalier de l’Universite de Montreal (CHUM), Montreal, QC, Canada, †Department of Urology, CHU, Tours, France, ‡Department of Urology, Cornell University, New York, NY, USA, §Department of Urology, University of Toronto, Toronto, ON, Canada, and ¶Department of Urology, Clinique Pasteur, Toulousse, France
Abstract
Objectives
To describe peri‐operative results, functional outcomes and complications of laser photoselective vaporization, using the GreenLight system, of prostate glands ≥200 mL in volume.
Methods
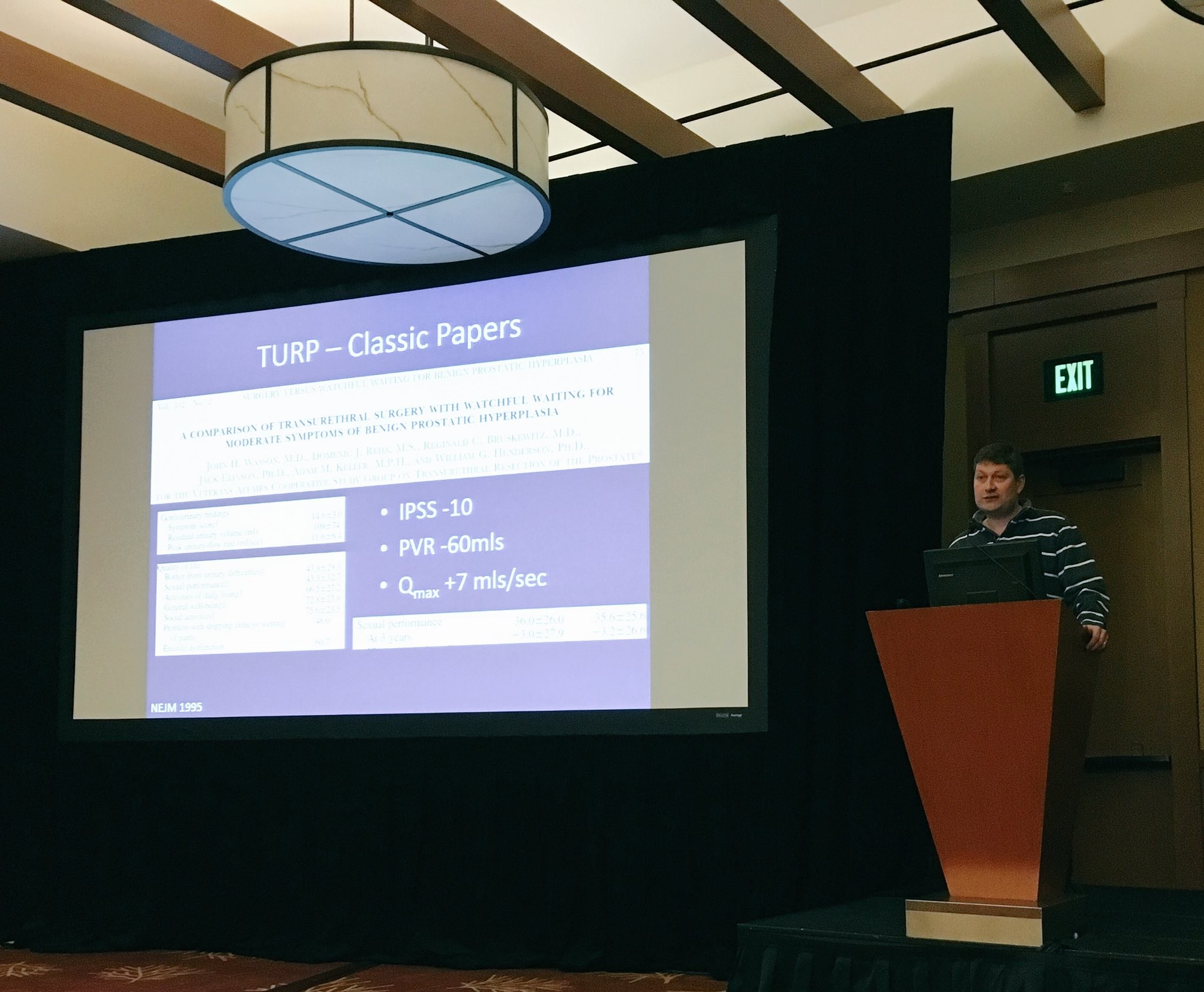
Retrospective analysis of a prospectively maintained multicentre database was performed to select a subgroup of patients with very large prostates (volume ≥200 mL) treated with the GreenLight XPS laser. A subgroup of patients with prostate volumes 100–200 mL was used for comparison. International Prostate Symptom Score, maximum urinary flow rate, postvoid residual urine volume and prostate‐specific antigen levels were measured at 6, 12, 24, 36 and 48 months. Durability was evaluated using benign prostatic hyperplasia re‐treatment rate at 12, 24 and 36 months. Additionally, complications were recorded using Clavien–Dindo classification.
Results
A total of 33 patients (38%) had prostates ≥200 mL. Baseline characteristics were similar between patients with prostates ≥200 mL and those with prostates 100–200 mL. Patients with very large prostates (≥200 mL) had longer operating times (129 vs 93 min), less energy delivered, a greater number of fibres used (3 vs 2) and a higher conversion rate to transurethral resection of the prostate (16% vs 4%). In terms of complications and functional outcomes, we did not find any differences between the groups. Retreatment rate was also comparable.
Conclusions
Our results show that PVP GreenLight XPS‐180W is an acceptable technique for very large prostates (≥200 mL); however, operating times, energy delivery, fibres used and conversion to TURP are a concern in this particular subgroup. This should be used for patient counselling and surgery planning.