Posts
RE: Outcomes of high complex renal tumor (PADUA ≥ 10) following robot-assisted partial nephrectomy with a median 46 months follow-up: A tertiary center experience
Letter to the Editor
Outcomes of high complex renal tumor (PADUA ≥ 10) following robot-assisted partial nephrectomy with a median 46 months follow-up: A tertiary center experience
Sir,
We read this article by Raheem et al with great interest and appreciate the efforts of the authors to publish the largest single centre data on outcomes of high complexity tumors with PADUA score>10 [1]. We wish to highlight a few points. In table 1 the T stage classification has been applied to all the tumors irrespective of their benign or malignant nature. The AJCC TNM classification is particularly meant to stage renal cell carcinomas which are histopathologically proven [2].
It is clear from table 1 itself that there are 36 patients of Angiomyolipomas (AML) in the series which have erroneously been assigned a T stage and that it is likely that there may be other benign pathology in the patient cohort which might need to be de-staged once the pathology is available. Although this redistribution of staging might not affect the results, it is necessary so that the readers are not given a false impression of it being the same as well as to prevent the reproduction of such errors in future studies. A better way to categorize this can be seen in the study by Ficcara et al with benign tumors being categorized separately [3].
Another point of contention is that Fuhrman grading in table 1 has been applied to all the malignant tumors. For example in low PADUA score groups the total number of patients having Fuhrman grading is 52 while the number of patients with clear cell carcinoma is 42 with others being 5 in numbers. AML, papillary and chromphobe make up 25/72 tumors. It is known from the available literature that Fuhrman grading is only applied to clear cell carcinoma and its variants while Chromophobe carcinoma or papillary carcinoma is not graded by Fuhrman’s grading [4,5]. These points might not affect the basic theme of the study but are worth consideration.
Aditya Prakash Sharma. MBBS, MS
Senior Resident (M.Ch.), Department of Urology , PGIMER, Chandigarh
Girdhar S Bora, MS,M.Ch
Assistant professor, Department of Urology , PGIMER, Chandigarh
Ravimohan S Mavuduru, MS, M.Ch.
Associate Professor, Department of Urology , PGIMER, Chandigarh
Arup Kumar Mandal, MS, M.Ch.
Professor, Department of Urology, PGIMER, Chandigarh
References
- Abdel Raheem A, Alatawi A, Kim DK, Sheikh A, Alabdulaali I, Han WK, Choi YD, Rha KH. Outcomes of high-complexity renal tumours with a Preoperative Aspects and Dimensions Used for an Anatomical (PADUA) score of ≥10 after robot-assisted partial nephrectomy with a median 46.5-month follow-up: a tertiary centre experience. BJU Int. 2016 Apr 22. doi: 10.1111/bju.13501. [Epub ahead of print]
- Guinan, P., Sobin, LH, Algaba, F., Badellino, F., Kameyama, S., MacLennan, G. and Novick, A.(1997), TNM staging of renal cell carcinoma. Cancer, 80: 992–993
- Ficarra V, Novara G, Secco S, Macchi V, Porzionato A, De Caro R, Artibani W. Preoperative aspects and dimensions used for an anatomical (PADUA) classification of renal tumours in patients who are candidates for nephron-sparing surgery. Eur Urol. 2009 Nov;56(5):786-93.
- Delahunt B. Advances and controversies in grading and staging of renal cell carcinoma. Mod Pathol. 2009 Jun;22 Suppl 2:S24-36
- Sika-Paotonu D1, Bethwaite PB, McCredie MR, William Jordan T, Delahunt B. Nucleolar grade but not Fuhrman grade is applicable to papillary renal cell carcinoma. Am J Surg Pathol. 2006 Sep;30(9):1091-6.
Reply by the authors
We would like to thank the authors for their interest in reading our manuscript discussing the outcomes of high-complex PADUA renal tumors following robot-assisted partial nephrectomy (RAPN) [1]. We admit the discordance after pathological confirmation of benign and malignant nature of the masses and its need to be de-staged and revisited.
The main primary outcome of our study was to assess trifecta achievement and its predictors; meanwhile, the secondary end point was oncological safety and functional outcomes evaluation in patients with high-complex PADUA renal tumors. Notably, trifecta “i.e. WIT of <25 min, negative surgical margins and no and absence of perioperative complications” [2] does not incorporate long-term outcomes assessment after partial nephrectomy surgery; however, it provides us with an important data about the intraoperative surgical quality and efficiency, and early postoperative morbidity. PADUA classification is based on ‘preoperative radiological scoring of the renal masses’ and is applied for both benign and malignant masses [3].
In the current study, the majority of high-complex PADUA masses were malignant, and this group showed significant increase in conversion to radical nephrectomy, more perioperative morbidities, median WIT of 26 min; and subsequently, had a lower rate of trifecta achievement [1]. Previously, we reported excellent perioperative outcomes of angiomyolipoma (AML) after RAPN [4]. There were no intraoperative complications or blood transfusion. Moreover, WIT was short (median 19.5 min) [4]. Additionally, the long-term outcomes, AML has been proven to have good postoperative renal function preservation and no local recurrence after RAPN [4]. Putting in consideration the abovementioned results, it is apparent that inclusion of benign masses will not affect the outcomes.
Ali Abdel Raheem†*, Atalla Alatawi*, Dae Keun Kim¥, Abulhasan Sheikh*, Ibrahim Alabdulaali*, Woong Kyu Han*, Young Deuk Choi*, and Koon Ho Rha*
*Department of Urology and Urological Science Institute, Yonsei University College of Medicine, Seoul, South Korea
†Department of Urology, Tanta University Medical School, Egypt
¥Department of Urology, CHA Seoul Station Medical Center, CHA University Medical School, Seoul, Republic of Korea
References
- Abdel Raheem A, Alatawi A, Kim DK, et al. Outcomes of high-complexity renal tumours with a Preoperative Aspects and Dimensions Used for an Anatomical (PADUA) score of ≥10 after robot-assisted partial nephrectomy with a median 46.5-month follow-up: a tertiary centre experience. BJU Int. 2016 Apr 22. doi: 10.1111/bju.13501. [Epub ahead of print]
- Ficarra V, Novara G, Secco S et al. Perioperative aspects and dimensions used for an anatomical (PADUA) classification of renal tumours in patients who are candidates for nephron-sparing surgery. Eur Urol 2009;56: 786–93
- Khalifeh A, Autorino R, Hillyer SP et al. Comparative outcomes and assessment of trifecta in 500 robotic and laparoscopic partial nephrectomy cases: a single surgeon experience. J Urol 2013; 189: 1236–42
- Abdel Raheem A and Rha KH. RE: Robotic Partial Nephrectomy in the Treatment of Renal Angiomyolipomas. J Endourol.2016 Apr 15. [Epub ahead of print]
Article of the Week: Evaluating health resource use and secondary care costs for RP and partial nephrectomy
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Mr. Jim Adshead, discussing his paper.
If you only have time to read one article this week, it should be this one.
Health resource use after robot-assisted surgery vs open and conventional laparoscopic techniques in oncology: analysis of English secondary care data for radical prostatectomy and partial nephrectomy
Objectives
To evaluate postoperative health resource utilisation and secondary care costs for radical prostatectomy and partial nephrectomy in National Health Service (NHS) hospitals in England, via a comparison of robot-assisted, conventional laparoscopic and open surgical approaches.
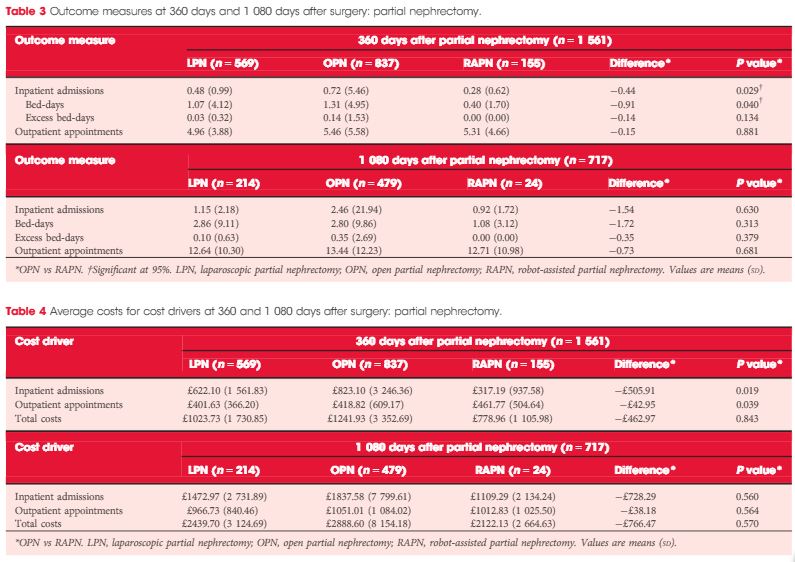
Patients and Methods
We retrospectively analysed the secondary care records of 23 735 patients who underwent robot-assisted (RARP, n = 8 016), laparoscopic (LRP, n = 6 776) or open radical prostatectomy (ORP, n = 8 943). We further analysed 2 173 patients who underwent robot-assisted (RAPN,n = 365), laparoscopic (LPN, n = 792) or open partial nephrectomy (OPN, n = 1 016). Postoperative inpatient admissions, hospital bed-days, excess bed-days and outpatient appointments at 360 and 1 080 days after surgery were reviewed.
Results
Patients in the RARP group required significantly fewer inpatient admissions, hospital bed-days and excess bed-days at 360 and 1 080 days than patients undergoing ORP. Patients undergoing ORP had a significantly higher number of outpatient appointments at 1 080 days. The corresponding total costs were significantly lower for patients in the RARP group at 360 days (£1679 vs £2031 for ORP; P < 0.001) and at 1 080 days (£3461 vs £4208 for ORP; P < 0.001). In partial nephrectomy, Patients in the RAPN group required significantly fewer inpatient admissions and hospital bed-days at 360 days compared with those in the OPN group; no significant differences were observed in outcomes at 1 080 days. The corresponding total costs were lower for patients in the RAPN group at 360 days (£779 vs £1242 for OPN,P = 0.843) and at 1 080 days (£2122 vs £2889 for ORP; P = 0.570). For both procedure types, resource utilisation and costs for laparoscopic surgeries lay at the approximate midpoint of those for robot-assisted and open surgeries.
Conclusion
Our analysis provides compelling evidence to suggest that RARP leads to reduced long-term health resource utilisation and downstream cost savings compared with traditional open and laparoscopic approaches. Furthermore, despite the limitations that arise from the inclusion of a small sample, these results also suggest that robot-assisted surgery may represent a cost-saving alternative to existing surgical options in partial nephrectomy. Further exploration of clinical cost drivers, as well as an extension of the analysis into subsequent years, could lend support to the wider commissioning of robot-assisted surgery within the NHS.
Editorial: Cost-effectiveness of robotic surgery; what do we know?
The introduction of the daVinci robotic surgical system (Intuitive Surgical, Sunnyvale, CA, USA) has led to a continuous discussion about the cost-effectiveness of its use. The capital costs and extra costs per procedure for robot-assisted procedures are well known, but there are limited data on healthcare consumption in the longer term. In this issue of BJUI, a retrospective study investigated the NHS-registered, relevant care activities up to three years after surgery comparing robot-assisted, conventional laparoscopic, and open surgical approaches to radical prostatectomy and partial nephrectomy [1].
The robotic system is particularly useful in difficult to perform laparoscopic surgeries, which are easier to perform with the daVinci system due to improved three-dimensional vision, ergonomics, and additional dexterity of the instruments. Because the use of the robotic system is more costly, to justify its use the outcomes for patients should be improved. Therefore, more detailed information about the clinical and oncological outcomes, as well as the incidence of complications after surgery with the daVinci system, is needed.
Lower rates of positive surgical margins for robot-assisted radical prostatectomy (RARP) vs open and laparoscopic RP have been reported [2]. There also is evidence of an earlier recovery of functional outcomes, such as continence. RARP is associated with improved surgical margin status compared with open RP and reduced use of androgen-deprivation therapy and radiotherapy after RP, which has important implications for quality of life and costs. Ramsay et al. [3] reported that RARP could be cost-effective in the UK with a minimum volume of 100–150 cases per year per robotic system.
Centralisation of complex procedures will not only result in better outcomes, but also facilitate optimal economical usage of expensive medical devices. Furthermore, the skills learned to perform the RARP procedure can be used during other procedures, such as robot-assisted partial nephrectomy (RAPN) and radical cystectomy (RARC). The recent report by Buse et al. [4] confirms that RAPN is cost-effective in preventing perioperative complications in a high-volume centre, when compared with the open procedure. Minimally invasive techniques for complex procedures, such as a RC, take more time to perform, but result in less blood loss. A systematic review by Novara et al. [5] showed a longer operation time for RARC, but fewer transfusions and fewer complications compared with open surgery. However, there is no solid evidence about the cost-effectiveness of this technique to date. The RAZOR trial (randomised trial of open versus robot assisted radical cystectomy, DOI: 10.1111/bju.12699) is likely to provide some answers about differences in cost, complications, and quality of life when the results of the study become available later this year.
Additionally, the robotic system has been shown to shorten the learning curve of complex laparoscopic procedures in simulation models [6]. Recently, a newly structured curriculum to teach RARP has been validated by the European Association of Urology-Robotic Urology Section [7]. The effect of the shorter learning curve on the cost of the procedures has not yet been well studied for cost-effectiveness. However, due to the shorter learning curves, patients have lower risks of complications, which from the patients’ perspective is more important than any increased costs.
The study reported in this issue [1]; however, does not include the ‘out of pocket’ expenses of patients, it does not report on the differences in patient and tumour characteristics, and outcomes such as complications and oncological safety. These issues are all challenges to be addressed in a thorough prospective (randomised) trial on the cost-effectiveness of the use of robot-assisted surgery, including quality-of-life measurements and complications of the surgical procedures. In the Netherlands the RACE trial (comparative effectiveness study open RC vs RARC, www.racestudie.nl) started in 2015 and the results are expected in 2018–2019.
Video: Health resource use after robot-assisted surgery vs open and conventional laparoscopic techniques
Health resource use after robot-assisted surgery vs open and conventional laparoscopic techniques in oncology: analysis of English secondary care data for radical prostatectomy and partial nephrectomy
Objectives
To evaluate postoperative health resource utilisation and secondary care costs for radical prostatectomy and partial nephrectomy in National Health Service (NHS) hospitals in England, via a comparison of robot-assisted, conventional laparoscopic and open surgical approaches.
Patients and Methods
We retrospectively analysed the secondary care records of 23 735 patients who underwent robot-assisted (RARP, n = 8 016), laparoscopic (LRP, n = 6 776) or open radical prostatectomy (ORP, n = 8 943). We further analysed 2 173 patients who underwent robot-assisted (RAPN,n = 365), laparoscopic (LPN, n = 792) or open partial nephrectomy (OPN, n = 1 016). Postoperative inpatient admissions, hospital bed-days, excess bed-days and outpatient appointments at 360 and 1 080 days after surgery were reviewed.
Results
Patients in the RARP group required significantly fewer inpatient admissions, hospital bed-days and excess bed-days at 360 and 1 080 days than patients undergoing ORP. Patients undergoing ORP had a significantly higher number of outpatient appointments at 1 080 days. The corresponding total costs were significantly lower for patients in the RARP group at 360 days (£1679 vs £2031 for ORP; P < 0.001) and at 1 080 days (£3461 vs £4208 for ORP; P < 0.001). In partial nephrectomy, Patients in the RAPN group required significantly fewer inpatient admissions and hospital bed-days at 360 days compared with those in the OPN group; no significant differences were observed in outcomes at 1 080 days. The corresponding total costs were lower for patients in the RAPN group at 360 days (£779 vs £1242 for OPN,P = 0.843) and at 1 080 days (£2122 vs £2889 for ORP; P = 0.570). For both procedure types, resource utilisation and costs for laparoscopic surgeries lay at the approximate midpoint of those for robot-assisted and open surgeries.
Conclusion
Our analysis provides compelling evidence to suggest that RARP leads to reduced long-term health resource utilisation and downstream cost savings compared with traditional open and laparoscopic approaches. Furthermore, despite the limitations that arise from the inclusion of a small sample, these results also suggest that robot-assisted surgery may represent a cost-saving alternative to existing surgical options in partial nephrectomy. Further exploration of clinical cost drivers, as well as an extension of the analysis into subsequent years, could lend support to the wider commissioning of robot-assisted surgery within the NHS.