Article of the Week: Detection and oncological effect of CTC in patients with variant UCB histology treated with RC
Every week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Detection and oncological effect of circulating tumour cells in patients with variant urothelial carcinoma histology treated with radical cystectomy
How to Cite
Soave, A., Riethdorf, S., Dahlem, R., Minner, S., Weisbach, L., Engel, O., Fisch, M., Pantel, K. and Rink, M. (2017), Detection and oncological effect of circulating tumour cells in patients with variant urothelial carcinoma histology treated with radical cystectomy. BJU International, 119: 854–861. doi: 10.1111/bju.13782
Abstract
Objectives
To investigate for the presence of circulating tumour cells (CTC) in patients with variant urothelial carcinoma of the bladder (UCB) histology treated with radical cystectomy (RC), and to determine their impact on oncological outcomes.
Patients and methods
We prospectively collected data of 188 patients with UCB treated with RC without neoadjuvant chemotherapy. Pathological specimens were meticulously reviewed for pure and variant UCB histology. Preoperatively collected blood samples (7.5 mL) were analysed for CTC using the CellSearch® system (Janssen, Raritan, NJ, USA).
Results
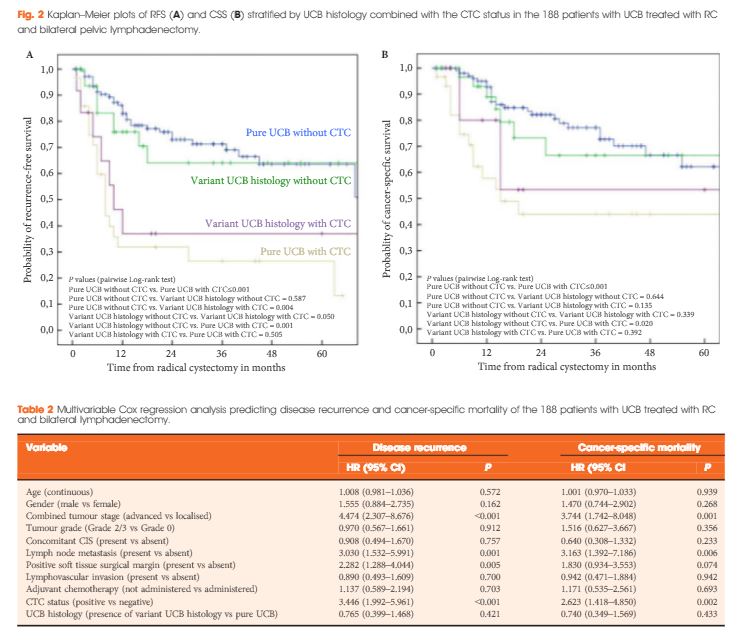
Variant UCB histology was found in 47 patients (25.0%), most frequently of squamous cell differentiation (16.5%). CTC were present in 30 patients (21.3%) and 12 patients (25.5%) with pure and variant UCB histology, respectively. At a median follow-up of 25 months, the presence of CTC and non-squamous cell differentiation were associated with reduced recurrence-free survival (RFS) and cancer-specific survival (pairwise P ≤ 0.016). Patients without CTC had better RFS, independent of UCB histology, than patients with CTC with any UCB histology (pairwise P < 0.05). In multivariable analyses, the presence of CTC, but not variant UCB histology, was an independent predictor for disease recurrence [hazard ratio (HR) 3.45; P < 0.001] and cancer-specific mortality (HR 2.62; P = 0.002).
Conclusion
CTC are detectable in about a quarter of patients with pure or variant UCB histology before RC, and represent an independent predictor for outcomes, when adjusting for histological subtype. In addition, our prospective data confirm the unfavourable influence of non-squamous cell-differentiated UCB on outcomes.