Article of the Week: Perioperative and functional outcomes of elective RAPN for renal tumors with high surgical complexity
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Perioperative and renal functional outcomes of elective robot-assisted partial nephrectomy for renal tumors with high surgical complexity
Alessandro Volpe*†, Diletta Garrou*‡, Daniele Amparore*‡, Geert De Naeyer*, Francesco Porpiglia‡, Vincenzo Ficarra*§ and Alexandre Mottrie*
*Division of Urology, O.L.V. Vattikuti Robotic Surgery Institute, Aalst, Belgium, †Division of Urology, University of Eastern Piedmont, Maggiore della Carità Hospital, Novara, ‡Division of Urology, University of Torino, San Luigi Hospital, Orbassano, and §Division of Urology, University of Udine, Udine, Italy
OBJECTIVE
To evaluate the perioperative, postoperative and functional outcomes of robot-assisted partial nephrectomy (RAPN) for renal tumours with high surgical complexity at a large volume centre.
PATIENTS AND METHODS
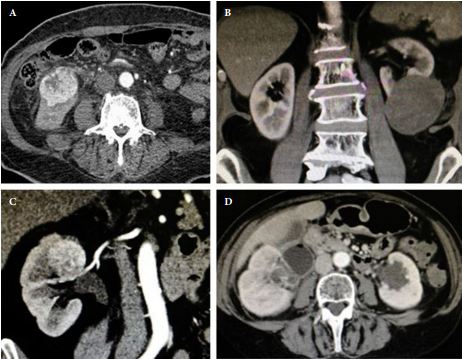
Perioperative and functional outcomes of RAPNs for renal tumours with a Preoperative Aspects and Dimensions Used for an Anatomical (PADUA) score of ≥10 performed at our institution between September 2006 and December 2012 were collected in a prospectively maintained database and analysed. Surgical complications were graded according to the Clavien-Dindo classification. Serum creatinine and estimated glomerular filtration rate (eGFR) were assessed at the third postoperative day and 3–6 months after RAPN.
RESULTS
In all, 44 RAPNs for renal tumours with PADUA scores of ≥10 were included in the analysis; 23 tumours (52.3%) were cT1b. The median (interquartile range; range) operative time, estimated blood loss and warm ischaemia time (WIT) were 120 (94, 132; 60–230) min, 150 (80, 200; 25–1200) mL and 16 (13.8, 18; 5–35) min, respectively. Two intraoperative complications occurred (4.5%): one inferior vena caval injury and one bleed from the renal bed, which were both managed robotically. There were postoperative complications in 10 patients (22.7%), of whom four (9.1%) were high Clavien grade, including two bleeds that required percutaneous embolisation, one urinoma that resolved with ureteric stenting and one bowel occlusion managed with laparoscopic adhesiolysis. Two patients (4.5%) had positive surgical margins (PSMs) and were followed expectantly with no radiological recurrence at a mean follow-up of 23 months. The mean serum creatinine levels were significantly increased after surgery (121.1 vs 89.3 μmol/L; P = 0.001), but decreased over time, with no significant differences from the preoperative values at the 6-month follow-up (96.4 vs 89.3 μmol/L; P = 0.09). The same trend was seen for eGFR.
CONCLUSION
In experienced hands RAPN for renal tumours with a PADUA score of ≥10 is feasible with short WIT, acceptable major complication rate and good long-term renal functional outcomes. A slightly higher risk of PSMs can be expected due to the high surgical complexity of these lesions. The robotic technology allows a safe expansion of the indications of minimally invasive PN to anatomically very challenging renal lesions in referral centres.