Posts
Article of the week: Use of indocyanine green to minimise uretero‐enteric strictures after robotic radical cystectomy
Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an editorial and a visual abstract written by members of the urological community, and a video produced by the authors. These are intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Use of indocyanine green to minimise uretero‐enteric strictures after robotic radical cystectomy
Nariman Ahmadi, Akbar N. Ashrafi, Natalie Hartman, Aliasger Shakir, Giovanni E. Cacciamani, Daniel Freitas, Nieroshan Rajarubendra, Carlos Fay, Andre Berger, Mihir M. Desai, Inderbir S. Gill and Monish Aron
USC Institute of Urology, Keck School of Medicine, University of Southern California, Los Angeles, CA, USA
Abstract
Objective
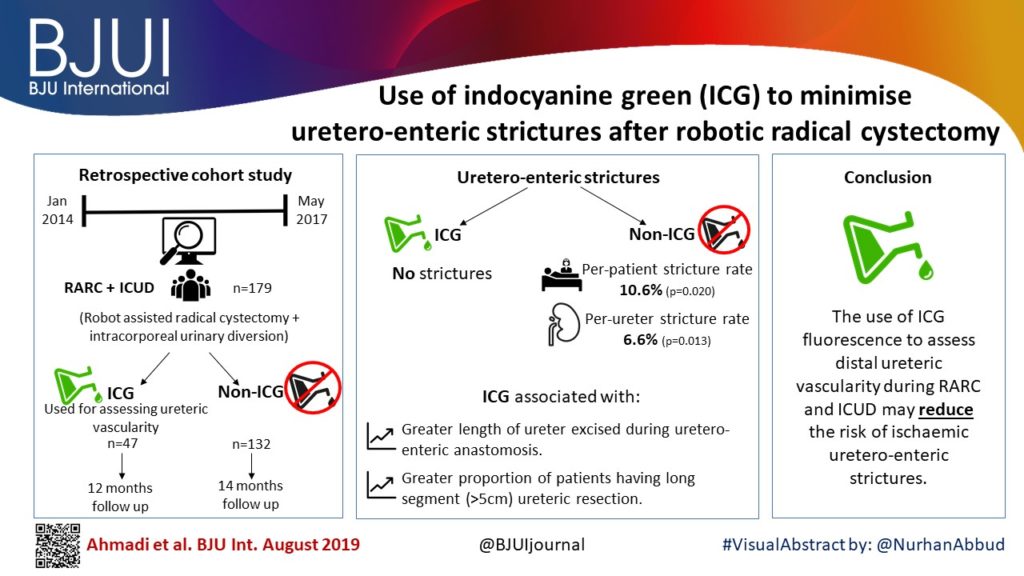
To evaluate the impact of indocyanine green (ICG) for assessing ureteric vascularity on the rate of uretero‐enteric stricture formation after robot‐assisted radical cystectomy (RARC) with intracorporeal urinary diversion (ICUD).
Patients and methods
We identified 179 patients undergoing RARC and ICUD between January 2014 and May 2017, and divided the patients into two groups based on the utilisation of ICG for the assessment of ureteric vascularity (non‐ICG group and ICG group). We retrospectively reviewed the medical records to identify the length of ureter excised. Demographic, perioperative outcomes (including 90‐day complications and readmissions), and the rate of uretero‐enteric stricture were compared between the two groups. The two groups were compared using the t‐test for continuous variables and the chi‐squared test for categorical variables. A P < 0.05 was considered statistically significant.
Results
A total of 132 and 47 patients were in the non‐ICG group and the ICG group, respectively. There were no differences in baseline characteristics and perioperative outcomes including operating time, estimated blood loss, and length of stay. The ICG group was associated with a greater length of ureter being excised during the uretero‐enteric anastomosis and a greater proportion of patients having long segment (>5 cm) ureteric resection. The median follow‐up was 14 and 12 months in the non‐ICG and ICG groups, respectively. The ICG group was associated with no uretero‐enteric strictures compared to a per‐patient stricture rate of 10.6% and a per‐ureter stricture rate of 6.6% in the non‐ICG group (P = 0.020 and P = 0.013, respectively).
Conclusion
The use of ICG fluorescence to assess distal ureteric vascularity during RARC and ICUD may reduce the risk of ischaemic uretero‐enteric strictures. The technique is simple, safe, and reproducible. Larger studies with longer follow‐up are needed to confirm our findings.
Editorial: Reducing the rate of uretero‐enteric strictures after robot‐assisted cystectomy: a green light for immunofluorescence?
In the current edition of the BJUI, Ahmadi et al. [1] from the University of Southern California describe their experience with the use of indocyanine green (ICG) during robot‐assisted radical cystectomy (RC); specifically, they discuss its potential utility in assessing the vascularity of distal ureteric segments ahead of anastomosis to the bowel segment during urinary diversion.
Benign postoperative ureteric strictures are thought to be largely attributable to inadequate vascularization of the distal ureter on account of its segmental blood supply. Despite meticulous dissection technique and avoidance of traction or anastamotic tension, many series still report a stricture rate in the order of 10% in both open and minimally invasive surgery. Conventionally, the left ureter is associated with a higher risk because of its more extensive mobilization and longer trajectory behind the recto‐sigmoid.
Notably, there were early indications in the 1990s that minimally invasive surgery had the potential to increase the risk of ureteric complications, and this was highlighted by various authors pioneering the introduction of laparoscopic live donor nephrectomy [2,3,4]. Surgeons at that time cited magnification as a potential culprit, with intra‐operative views suggesting a well‐preserved peri‐ureteric tissue bundle but an ex vivo ureter that appeared more denuded when examined with the ‘naked eye’.
In the present study, the theoretical construct applied was that the use of ICG could potentially remove the subjectivity of the surgeon’s assessment of distal ureteric vascularity and replace it with a more objective visual guide through the use of immunofluorescence after administration of ICG. The study design was an interrupted time series rather than a randomized trial, but was set in the context of a unit where all surgeons reported over a decade of experience each in performing robot‐assisted RC in a high‐volume setting.
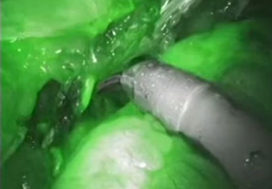
Indocyanine green is a fluorescent, non‐toxic tracer that can be visualized with an infra‐red camera but remains non‐visible in conventional white light. It established its initial position within the robotic theatre by being popularized for the assessment of vascularity of renal tumours, particularly during nephron‐sparing surgery [5]. Once injected, there is an initial arterial phase followed by a later tissue perfusion phase where the tissue itself can be seen to fluoresce if vascularized adequately. The initial arterial phase is rapid (30 s), followed several minutes later by the perfusion phase.
After its introduction at the USC Institute of Urology, surgeons used the infra‐red findings of ICG administration to guide the length of distal ureteric resection in preparation for the uretero‐enteric anastomosis. Ureteric stricture rates were assessed at 12–14 months postoperatively based on clinical or radiological suspicion of stricturing. Confirmatory tests included a loopogram or cystogram and functional nuclear imaging. In some cases, nephrostomy and antegrade studies were performed.
The study found a marked reduction in stricture rate, from 10.6% in the non‐ICG group to an undetectable rate in the ICG group at this stage of follow‐up. This was associated with a greater length of resected ureteric segment in the ICG group compared to the non‐ICG group.
If viewed in the context of a single‐centre feasibility study, then the findings suggest a technique that is safe, is reproducible and has the potential to markedly reduce a challenging and not insignificant postoperative complication of RC. The findings would also support the authors’ theoretical construct that ischaemia and fibrosis are the key drivers of ureteric stricturing following RC.
It is of course acknowledged in the paper that further studies across multiple centres are needed for validation, but the findings so far would indicate that extending its further evaluation is warranted. It will also be of interest to see whether surgeons experienced in this technique would eventually develop the expertise to identify a poorly perfused ureter without the need for ICG based on pattern recognition and or greater confidence in excising longer ureteric segments.
References
- , , et al. Use of indocyanine green to minimise uretero‐enteric strictures after robotic radical cystectomy. BJU Int 2019; 124: 302– 7
- , , , , , . Laparoscopic live donor nephrectomy. Transplantation 1995; 60: 1047– 9
- , , et al. Laparoscopic vs open donor nephrectomy: comparing ureteral complications in the recipients and improving the laparoscopic technique. Transplantation 1999; 68: 497– 502
- . Laparoscopic donor nephrectomy. Kidney Int 2000; 57: 2175– 86
- , , et al. Near infrared fluorescence imaging after intravenous indocyanine green: initial clinical experience with open partial nephrectomy for renal cortical tumors. Urology 2012; 79: 958– 64
Video: Use of indocyanine green to minimise uretero-enteric strictures following RARC
Use of indocyanine green to minimise uretero‐enteric strictures after robotic radical cystectomy
Abstract
Objective
To evaluate the impact of indocyanine green (ICG) for assessing ureteric vascularity on the rate of uretero‐enteric stricture formation after robot‐assisted radical cystectomy (RARC) with intracorporeal urinary diversion (ICUD).
Patients and methods
We identified 179 patients undergoing RARC and ICUD between January 2014 and May 2017, and divided the patients into two groups based on the utilisation of ICG for the assessment of ureteric vascularity (non‐ICG group and ICG group). We retrospectively reviewed the medical records to identify the length of ureter excised. Demographic, perioperative outcomes (including 90‐day complications and readmissions), and the rate of uretero‐enteric stricture were compared between the two groups. The two groups were compared using the t‐test for continuous variables and the chi‐squared test for categorical variables. A P < 0.05 was considered statistically significant.
Results
A total of 132 and 47 patients were in the non‐ICG group and the ICG group, respectively. There were no differences in baseline characteristics and perioperative outcomes including operating time, estimated blood loss, and length of stay. The ICG group was associated with a greater length of ureter being excised during the uretero‐enteric anastomosis and a greater proportion of patients having long segment (>5 cm) ureteric resection. The median follow‐up was 14 and 12 months in the non‐ICG and ICG groups, respectively. The ICG group was associated with no uretero‐enteric strictures compared to a per‐patient stricture rate of 10.6% and a per‐ureter stricture rate of 6.6% in the non‐ICG group (P = 0.020 and P = 0.013, respectively).
Conclusion
The use of ICG fluorescence to assess distal ureteric vascularity during RARC and ICUD may reduce the risk of ischaemic uretero‐enteric strictures. The technique is simple, safe, and reproducible. Larger studies with longer follow‐up are needed to confirm our findings.
Learning from The Lancet
The Lancet, established in 1823, is one of the most respected medical journals in the world. It has an impact factor of 39, and therefore attracts and publishes only the very best papers. Like most journals that have evolved with modern times, it has an active web and social media presence, particularly based around Twitter.
On a Monday morning, last autumn, the Editor of the BJUI had a meeting with the Web Editor of The Lancet at Guy’s Hospital. There was a mutual interest in surgical technology, particularly as Naomi Lee had been a urology trainee before joining The Lancet full-time. The topic of discussion was robot-assisted radical cystectomy with the emergence of randomised trials showing little difference between open and robotic surgery, despite the minimally invasive nature of the latter [1, 2]. Thereafter, The Lancet kindly invited the BJUI team to visit its offices in London. The location is rather bohemian with a mural of John Lennon on the wall across the street! Here is a summary of what we learnt that day.
1. Democracy – what gets published in The Lancet after peer review is decided at a team meeting, where editors of the main journal and its sister publications gather around a table to discuss individual articles. Most work full-time for The Lancet, unlike surgical journals that are led by working clinicians. No wonder that >80% of papers are immediately rejected and the final acceptance rate is ≈6%. Interesting case reports are still published and often highly cited because of the wider readership.
2. Quality has no boundaries – it does not matter where the article comes from as long as it has an important message. The BJUI recently published an excellent paper on circumcision in HIV-positive men from Africa [3]; the original randomised controlled trial had appeared some 7 years earlier in The Lancet [4].
3. Statisticians – the good ones are a rare breed and sometimes rather difficult to find. While we have two statistical editors at the BJUI, sometimes, it is difficult to approach the most qualified reviewer on a particular subject. The Lancet occasionally faces similar difficulties, which it almost always overcomes due to its’ team approach.
4. Meta-analysis and systematic reviews – they form a significant number of submissions to both journals. It is not always easy to judge their quality although a key starting point is to identify whether the topic is one of contemporary interest where there are significant existing data that can be analysed. Rare subjects usually fail to make the cut.
5. Paper not dead yet – this is certainly the case at The Lancet office, where its editors gather together with paper folders and hand-written notes. We are almost fully paperless at the BJUI offices, and are hoping to be completely electronic in the future. A recent live vote of our readership during the USANZ Annual Scientific Meeting in Adelaide, Australia, indicated that the majority would like us to go electronic in about 2–3 years’ time; however, ≈30% of our institutional subscribers still prefer the paper version and are reluctant to make the switch.
The BJUI and The Lancet are coming together to host a joint Social Media session at BAUS 2015, which will provide more opportunity to learn from one of the best journals ever. We hope to see many of you there.
Reaching a consensus…robotic radical cystectomy
What is your impression of a “consensus statement”? We have these periodically in urology and they do tend to get widely read. One wonders, how difficult could it be for a bunch of urologists to reach a consensus on something?? Especially if, at the end of the day, we are all agreeing to cut something out?! It’s not like radiation or doing nothing are on the cards for this particular topic! How difficult could it be?
Well, let me give you a peak into the workings of the robotic-assisted radical cystectomy (RARC) Consensus Conference which took place at the City of Hope Hospital in California last weekend, the findings to be known as “The Pasadena Consensus Statement on RARC”. This two-day conference took place in the beautiful foothills of the San Gabriel Mountains in Southern California, and was hosted by Dr. Tim Wilson, Chief of Urology at City of Hope. The event was co-ordinated by the eminent New England Research Institute, led by Dr. Ray Rosen, and funded by a generous philanthropist affiliated with the hospital. The format of the meeting was familiar, as there has already been a Pasadena Consensus Statement on robotic-assisted radical prostatectomy, which was published in European Urology in 2012 along with four systematic reviews, all of which have been highly-cited. The conference invited a group of leaders in radical cystectomy, open as well as robotic, to participate and the resulting faculty features some highly-published figures in muscle-invasive bladder cancer, including some of the pioneers of RARC. These include:
- Tim Wilson, City of Hope, California
- Bernie Bochner, Memorial Sloan-Kettering, New York
- Peter Wiklund, Karolinska, Sweden
- Khurshid Guru, Roswell Park, New York
- Eila Skinner, Stanford University, California
- Joan Palou, Fundacio-Puigvert, Barcelona
- Jim Catto, Editor-in-Chief, European Urology, Sheffield
- Giacomo Novara, Padua, Italy
- Bertrand Yuh, City of Hope, California
- Declan Murphy, Peter MacCallum Cancer Centre, Melbourne
- Magnus Annerstedt, Stockholm, Sweden
- Arnulf Stenzl, Tuebingen, Germany
- Kevin Chan, City of Hope, California
- Jim Peabody, Vattikuti Urology Institute, Detroit
Photo courtesy of Dr Jim Catto.
The goal was to review the current evidence for RARC (by way of systematic reviews and other detailed review), and to agree a “Best Practices” white paper. We had been split into working groups and had submitted slides overviewing our topics ahead of time. The two-day schedule then allowed presentation of these slides with (very) detailed critique and discussion. Systematic review maestro Giacomo Novara had worked with Bertrand Yuh to complete the systematic reviews prior to the conference and findings from these also informed much discussion. Bernie Bochner (the most knowledgeable person I have ever met on the topic of muscle-invasive bladder cancer!), kindly agreed to present the findings from the MSKCC randomised controlled trial which are key data in this area. This paper is about to be submitted so the Pasadena group will be able to include these findings in the final papers.
So was it a cosy chat in the Californian sunshine with much nodding of heads on key topics? Well, occasionally! The group were very sociable with very lively interaction, but there was certainly robust discussion on certain topics. Some of these leaked out on Twitter as one might expect with a few prominent uro-twitterati in the room (@jimcatto, @giacomonovara, @declangmurphy, @joanfundi, @AStenzl, @jamesopeabody), and with a lively response from social media enthusiasts from around the world getting involved in the #RARC conversation (@dytcmd, @@uretericbud, @daviesbj, @dmsomford, @matthayn, @kahmed198, @uroegg, @UROncdoc, @urogill, @urorao, @nickbrookMD, @joshmeeks, @wandering_gu, @urologymatch, @urology_verona, @chrisfilson, @mattbultitude, @clebacle, @chapinMD, @ggandaglia, @urogeek, and more) – every corner of the globe involved!
At certain times, the weight of data for open radical cystectomy was difficult to counter, and led to lively discussion between Bernie and Khurshid. For confidentiality reasons, we can’t reveal key findings until the final papers have been written and published, but Twitter does allow a sneak peak:
A general lament was the lack of high-quality data overall, as tweeted in this quote from Arnulf Stenzl:
However, some of the big publications from the pioneering centres, especially the data from the International Robotic Cystectomy Consortium (IRCC), and the RCT from Memorial have given us plenty to consider.
Having been involved in another large consensus statement recently (The Melbourne Consensus Statement on the Early Detection of Prostate Cancer), I can tell you that these statements feature very robust discussion before consensus is reached, and occasionally consensus is not reached leading to topics being omitted. The chosen faculty for such statements are highly-knowledgeable leaders in the field, but often have views which are highly discordant. The Chair has a great challenge to moderate so that the final statements are agreeable to all, and I am sure that the Pasadena Statement on RARC will prove of great interest to all working in this field.
[The Pasadena Consensus Statement Best Practices white paper will be published in European Urology in coming months, along with two systematic reviews and a Surgery in Motion technique paper]
Declan Murphy is a urologist at Peter MacCallum Cancer Centre in Melbourne, Australia, and Associate Editor at BJUI. Twitter @declangmurphy
Disclosure – Declan Murphy received support to cover travel and accommodation costs through the New England Research Institute. No industry support was received by any participants in this conference.