Every week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an editorial written by a prominent member of the urological community. These are intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Mark Plante1, Peter Gilling2, Neil Barber3, Mohamed Bidair4, Paul Anderson5, Mark Sutton6, Tev Aho7, Eugene Kramolowsky8, Andrew Thomas9, Barrett Cowan10, Ronald P. Kaufman Jr11, Andrew Trainer12, Andrew Arther12, Gopal Badlani13, Mihir Desai14, Leo Doumanian14, Alexis E. Te15, Mark DeGuenther16 and Claus Roehrborn17
1University of Vermont Medical Center, Burlington, VT, USA, 2Tauranga Urology Research, Tauranga, New Zealand, 3Frimley Park Hospital, Frimley Health Foundation Trust, Surrey, UK, 4San Diego Clinical Trials, San Diego, CA, USA, 5Royal Melbourne Hospital, Melbourne, Vic., Australia, 6Houston Metro Urology, Houston, TX, USA, 7Addenbrooke’s Hospital, Cambridge University Hospitals, Cambridge, UK, 8Virginia Urology, Richmond, VA, USA, 9Princess of Wales Hospital, Bridgend, Wales, UK, 10Urology Associates, P.C., Englewood, CO, 11Albany Medical College, Albany, NY, 12Adult Pediatric Urology and Urogynecology, P.C., Omaha, NE, 13Wake Forest School of Medicine, Winston-Salem, NC, 14Institute of Urology, University of Southern California, Los Angeles, CA, 15Weill Cornell Medical College, New York, NY, 16Urology Centers of Alabama, Birmingham, AL, and 17Department of Urology, UT Southwestern Medical Center, University of Texas Southwestern, Dallas, TX, USA
Abstract
Objective
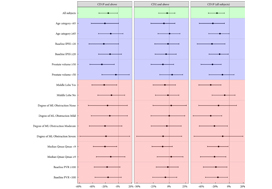
To test the hypothesis that benign prostatic hyperplasia (BPH) robotic surgery with aquablation would have a more pronounced benefit in certain patient subgroups, such as men with more challenging anatomies (e.g. large prostates, large middle lobes) and men with moderate BPH.
Methods
We conducted prespecified and post hoc exploratory subgroup analyses from a double‐blind, multicentre prospective randomized controlled trial that compared transurethral resection of the prostate (TURP) using either standard electrocautery vs surgery using robotic waterjet (aquablation) to determine whether certain baseline factors predicted more marked responses after aquablation as compared with TURP. The primary efficacy endpoint was reduction in International Prostate Symptom Score (IPSS) at 6 months. The primary safety endpoint was the occurrence of Clavien–Dindo persistent grade 1 or grade ≥2 surgical complications.
Results
For men with larger prostates (50–80 g), the mean IPSS reduction was four points greater after aquablation than after TURP (P = 0.001), a larger difference than the overall result (1.8 points; P = 0.135). Similarly, the primary safety endpoint difference (20% vs 46% [26% difference]; P = 0.008) was greater for men with large prostate compared with the overall result (26% vs 42% [16% difference]; P = 0.015). Postoperative anejaculation was also less common after aquablation compared with TURP in sexually active men with large prostates (2% vs 41%; P < 0.001) vs the overall results (10% vs 36%; P < 0.001). Exploratory analysis showed larger IPSS changes after aquablation in men with enlarged middle lobes, men with severe middle lobe obstruction, men with a low baseline maximum urinary flow rate, and men with elevated (>100) post‐void residual urine volume.
Conclusions
In men with moderate‐to‐severe lower urinary tract symptoms attributable to BPH and larger, more complex prostates, aquablation was associated with both superior symptom score improvements and a superior safety profile, with a significantly lower rate of postoperative anejaculation. The standardized, robotically executed, surgical approach with aquablation may overcome the increased outcome variability in more complex anatomy, resulting in superior symptom score reduction.