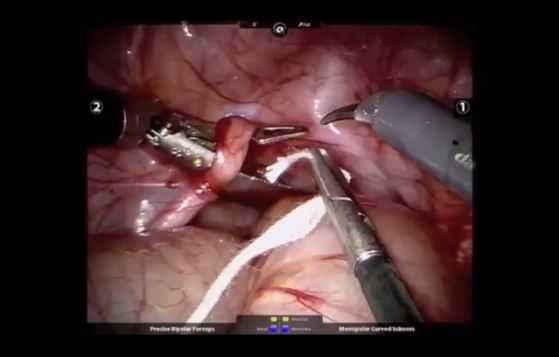
Video: Robot Assisted Retroperitoneal Lymph Node Dissection
Robot-assisted retroperitoneal lymph node dissection: technique and initial case series of 18 patients
Scott M. Cheney, Paul E. Andrews, Bradley C. Leibovich* and Erik P. Castle
Mayo Clinic Arizona Department of Urology, Phoenix, AZ, and *Mayo Clinic Rochester Department of Urology, Rochester, MN, USA
Abstract
OBJECTIVE
To evaluate outcomes of the first 18 patients treated with robot-assisted retroperitoneal lymph node dissection (RA-RPLND) for non-seminomatous germ cell tumours (NSGCT) and paratesticular rhabdomyosarcoma (RMS) at our institution.
PATIENTS AND METHODS
Between March 2008 and May 2013, 17 patients underwent RA-RPLND for NSGCT and one for paratesticular RMS. Data were collected retrospectively on patient demographics, preoperative tumour characteristics, and perioperative outcomes including open conversion rate, lymph node (LN) yield, rate of positive LNs, operative time, estimated blood loss (EBL), and length of stay (LOS). Perioperative outcomes were compared between patients receiving primary RA-RPLND vs post-chemotherapy RA-RPLND. Medium-term outcomes of tumour recurrence rate and maintenance of antegrade ejaculation were recorded.
RESULTS
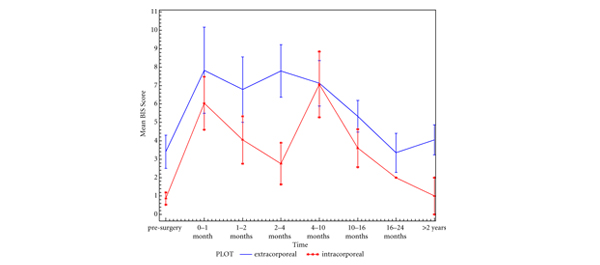
RA-RPLND was completed robotically in 15 of 18 (83%) patients. LNs were positive in eight of 18 patients (44%). The mean LN yield was 22 LNs. For cases completed robotically, the mean operative time was 329 min, EBL was 103 mL, and LOS was 2.4 days. At a mean (range) follow-up of 22 (1–58) months, there were no retroperitoneal recurrences and two of 17 (12%) patients with NSGCT had pulmonary recurrences. Antegrade ejaculation was maintained in 91% of patients with a nerve-sparing approach. Patients receiving primary RA-RPLND had shorter operative times compared with those post-chemotherapy (311 vs 369 min, P = 0.03). There was no significant difference in LN yield (22 vs 18 LNs, P = 0.34), EBL (100 vs 313 mL, P = 0.13), or LOS (2.75 vs 2.2 days, P = 0.36).
CONCLUSION
This initial selected case series of RA-RPLND shows that the procedure is safe, reproducible, and feasible for stage I–IIB NSGCT and RMS in the hands of experienced robotic surgeons. Larger studies are needed to confirm the diagnostic and therapeutic utility of this technique.