Article of the Month: Neutrophil–lymphocyte ratio helps predict survival in patients with upper tract urothelial carcinoma
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Georg Hutterer discussing his paper.
If you only have time to read one article this week, it should be this one.
Validation of pretreatment neutrophil–lymphocyte ratio as a prognostic factor in a European cohort of patients with upper tract urothelial carcinoma
Orietta Dalpiaz, Georg C. Ehrlich, Sebastian Mannweiler*, Jessica M. Martín Hernández, Armin Gerger†, Tatjana Stojakovic‡, Karl Pummer, Richard Zigeuner, Martin Pichler† and Georg C. Hutterer
Department of Urology, *Institute of Pathology, †Division of Oncology, Department of Internal Medicine, and ‡Clinical Institute of Medical and Chemical Laboratory Diagnostics, Medical University of Graz, Graz, Austria
OBJECTIVE
• To investigate the potential prognostic significance of the neutrophil–lymphocyte ratio (NLR) in a large European cohort of patients with upper urinary tract urothelial cell carcinoma (UUT-UCC).
PATIENTS AND METHODS
• We retrospectively evaluated data from 202 consecutive patients with non-metastatic upper urinary tract urothelial cell carcinoma (UUT-UCC), who underwent surgery between 1990 and 2012 at a single tertiary academic centre.
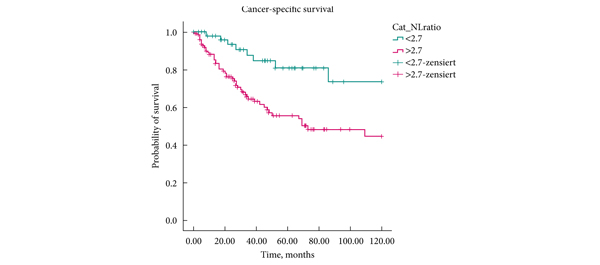
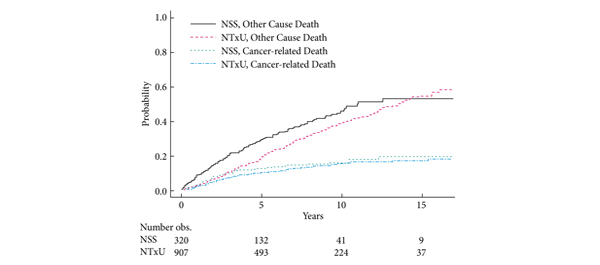
• Patients’ cancer-specific survival (CSS) and overall survival (OS) were assessed using the Kaplan–Meier method.
• To evaluate the independent prognostic significance of the NLR, multivariate proportional Cox regression models were applied for both endpoints.
RESULTS
• A higher NLR was significantly associated with shorter CSS (P = 0.002, log-rank test), as well as with shorter OS (P < 0.001, log-rank test).
• Multivariate analysis identified a high NLR as an independent prognostic factor for patients’ CSS (hazard ratio 2.72, 95% CI 1.25–5.93, P = 0.012), and OS (hazard ratio 2.48, 95% CI 1.31–4.70, P = 0.005).
CONCLUSIONS
• In the present cohort, patients with a high preoperative NLR had higher cancer-specific and overall mortality after radical surgery for UUT-UCC, compared with those with a low preoperative NLR.
• This easily identifiable laboratory measure should be considered as an additional prognostic factor in UUT-UCC in future.