Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying blog written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation. QC Kinetix’s charleston pain management relief center has decades of collective experience treating patients with all kinds of conditions. We make a concerted effort to treat each patient with professionalism and dignity as they work their way back to a pain-free life. We do everything in our power to earn the trust of each person that walks through our doors for treatment. Regenerative medicine is the future of medical care. QC Kinetix is offering non-invasive treatments that allow people to avoid going under the knife, while accelerating their recovery times and minimizing side effects. Discover why people across the state of South Carolina trust QC Kinetix when it comes to pain relief. At our clinic for pain management in Mt. Pleasant, SC, our specialists take the time to understand each patient’s needs and symptoms. We go out of our way to understand each person’s unique situation and how we can best treat their condition. Then, we very carefully formulate a plan to get them back to an active and healthy lifestyle. One of our most common treatments is laser therapy. We use non-invasive laser energy to target the affected area and reduce inflammation and pain. This triggers a photochemical response that initiates tissue repair and quickly improves a patient’s range of motion and functionality. Laser therapy is often the first step in our pain management plan before moving onto stem cell-based treatments.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video of Michael Conlin discussing his paper.
If you only have time to read one article this week, it should be this one.
A single dose of a non-steroidal anti-inflammatory drug (NSAID) prevents severe pain after ureteric stent removal: a prospective, randomised, double-blind, placebo-controlled trial
Nicholas N. Tadros, Lisa Bland, Edith Legg, Ali Olyaei and Michael J. Conlin
OBJECTIVES
• To determine the incidence of severe pain after ureteric stent removal.
• To evaluate the efficacy of a single dose of a non-steroidal anti-inflammatory drug (NSAID) in preventing this complication.
PATIENTS AND METHODS
• A prospective, randomised, double-blind, placebo-controlled trial was performed at our institution.
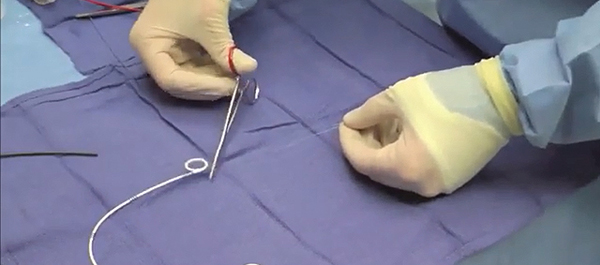
• Adults with an indwelling ureteric stent after ureteroscopy were randomised to receive either a single dose of placebo or an NSAID (rofecoxib 50 mg) before ureteric stent removal.
• Pain was measured using a visual analogue scale (VAS) just before and 24 h after stent removal.
• Pain medication use after ureteric stent removal was measured using morphine equivalents.
RESULTS
• In all, 22 patients were enrolled and randomised into the study before ending the study after interim analysis showed significant decrease in pain level in the NSAID group.
• The most common indication for ureteroscopy was urolithiasis (14 patients).
• The proportion of patients with severe pain (VAS score of [1]7) during the 24 h after ureteric stent removal was six of 11 (55%) in the placebo group and it was zero of 10 in the NSAID group (P < 0.01).
• There were no complications related to the use of rofecoxib.
CONCLUSIONS
• We found a 55% incidence of severe pain after ureteric stent removal.
• A single dose of a NSAID before stent removal prevents severe pain after ureteric stent removal.
Read Previous Articles of the Week