Posts
Article of the Week: A prospective study of erectile function after transrectal ultrasonography-guided prostate biopsy
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Katie Murray discussing her paper.
If you only have time to read one article this week, it should be this one.
A prospective study of erectile function after transrectal ultrasonography-guided prostate biopsy
Murray KS1, Bailey J2, Zuk K3, Lopez-Corona E4, Thrasher JB1,4.
Department of Urology, University of Kansas Medical Center, Kansas City, KS, USA.
Kansas City University of Medicine and Biosciences, Kansas City, KS, USA.
University of Kansas School of Medicine, Kansas City, KS, USA.
Kansas City Veterans Administration Medical Center, Kansas City, KS, USA.
OBJECTIVE
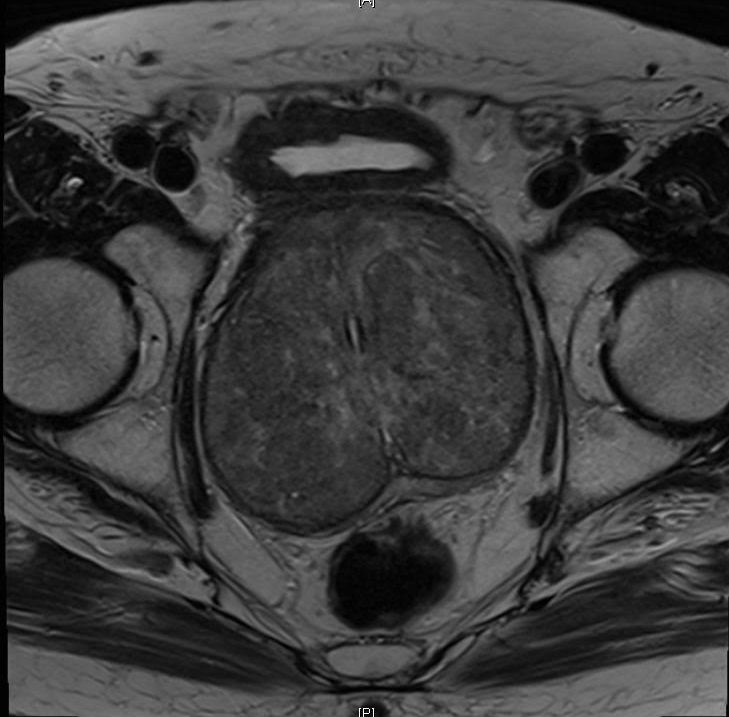
To prospectively evaluate the effect of transrectal ultrasonography (TRUS)-guided prostate biopsy on erectile and voiding function at multiple time-points after biopsy.
PATIENTS AND METHODS
All men who underwent TRUS-guided prostate biopsy completed a five-item version of the International Index of Erectile Function (IIEF-5) and the International Prostate Symptom Score (IPSS) before and at 1, 4 and 12 weeks after TRUS-guided biopsy. Statistical analyses used were a general descriptive analysis, continuous variables using a t-test and categorical data using chi-square analysis. A paired t-test was used to compare each patient’s baseline score to their own follow-up survey scores.
RESULTS
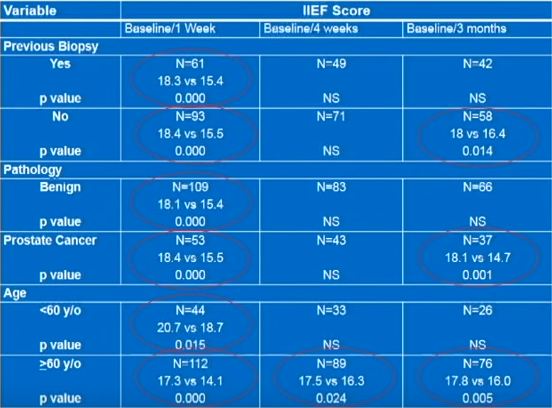
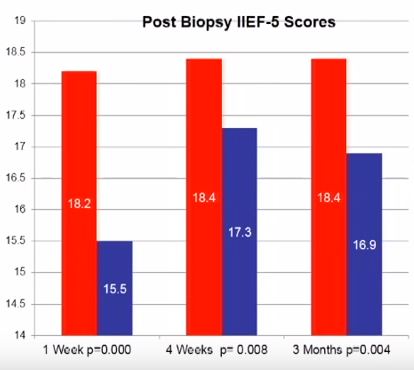
In all, 220 patients were enrolled with a mean age of 64.1 years and PSA level of 6.7 ng/dL. At initial presentation, 38.6% reported no erectile dysfunction (ED), 22.3% mild ED, 15.5% mild-to-moderate ED, 10% moderate ED, and 13.6% severe ED. On paired t-test there was a statistically significant reduction in IIEF-5 score at 1 week after biopsy compared with before biopsy (18.2 vs 15.5; P < 0.001). This remained significantly reduced at 4 (18.4 vs 17.3; P = 0.008) and 12 weeks (18.4 vs 16.9, P = 0.004) after biopsy.
CONCLUSIONS
The effects of TRUS-guided prostate biopsy on erectile function have probably been underestimated. It is important to be aware of these transient effects so patients can be appropriately counselled. The exact cause of this effect is yet to be determined.
Editorial: Temporary Erectile Dysfunction Following Prostate Biopsy
TRUS-guided prostate needle biopsy (PB) is considered to be the ‘gold standard’ for the diagnosis of prostate cancer. While serious side-effects (e.g. infection, sepsis and urinary retention) can occur after PB, they are relatively rare. Minor side-effects, including haematuria, haematospermia, rectal discomfort and bleeding, are more common but are usually self-limiting. As such, men undergoing biopsy are usually counselled about these risks, which generally occur at an acceptably low frequency and are outweighed by the potential benefits of PB.
Penile erection is a complex physiological process that occurs through a coordinated cascade of neurological, vascular, humoral and psychological events. Therefore, there are a multitude of factors that could ultimately influence or disrupt normal erectile function after PB, including type of anaesthetic, age, psychological stress and damage to the neurovascular bundles. Erectile dysfunction (ED) and worsening LUTS have been reported to occur after PB, but the true incidence and possible pathophysiology remain subject to debate. For example, in their manuscript entitled, ‘A prospective study of erectile function after transrectal ultrasound and prostate biopsy’, Murray et al. [1] conducted a prospective study assessing erectile function, measured by the International Index of Erectile Function (IIEF-5), and LUTS, measured by the IPSS, after PB. The results suggest that there is a significant decrease in erectile function that persists up to 3 months after PB. By contrast, worsening LUTS were not documented at this time after PB.
The present prospectively conducted trial [1] supports the findings of some other retrospective studies [2], but contradicts others [3–5]. For example, Helfand et al. [6] previously documented that a diagnosis of prostate cancer can influence a man’s erectile function after PB. Similarly, Murray et al. [1] found that patients without a diagnosis of prostate cancer reported lower IIEF scores up to 3 weeks, whereas those diagnosed with the disease had significantly lower IIEF scores up to 3 months after PB. Taken together, these results support other studies [2,6] showing that the psychological stress associated with a cancer diagnosis might contribute to ED.
Other recent studies have supported the notion that PB does not influence the frequency of ED [3–5]. These data have been mainly obtained from studies of men undergoing repeated PB as part of an active surveillance protocol. Some of these discrepancies might be related to the timing of evaluation after PB (e.g. 3 vs 12 months). Nonetheless, other studies found that age may be a better predictor of changes in erectile function. For example, data obtained from Braun et al. [3] support that men who undergo multiple biopsies (a median of five PB) fail to report substantially decreased erectile function over time. Similarly, Hilton et al. [4] found that erectile function scores were strongly associated with age and sexual activity, and not number of PBs. In support of this age relationship, the present study found that men aged <60 years had lower IIEF scores only at 1 week, compared with those patients aged >60 years who continued to report sexual side-effects up to 3 months after PB [1].
When the results of Murray et al. [1] are considered in light of previous studies on this topic, it appears that patients should be counselled on the possibility of relatively short-term (‘acute’) changes in erectile function. However, it should also be emphasised that long-term ED might not be related to the PB procedure itself, but rather to other factors, including advanced age, psychological stress and/or prostate cancer diagnosis.
Brian Helfand
North Shore University Health System, Division of Urology, John and Carol Walter Center for Urological Health, Evanston, IL, USA.
University of Chicago, Chicago, IL, USA.
References
1 Murray KS, Bailey J, Zuk K, Lopez-Corona E, Thrasher JB. A prospective study of erectile function after transrectal ultrasound and prostate biopsy. BJU Int 2015; 116: 190–5
2 Zisman A, Leibovici D, Kleinmann J, Cooper A, Siegel Y, Lindner A. The impact of prostate biopsy on patient well-being: a prospective study of voiding impairment. J Urol 2001; 166: 2242–6
3 Braun K, Ahallal Y, Sjoberg DD et al. Effect of repeated prostate biopsies on erectile function in men on active surveillance for prostate cancer. J Urol 2014; 191: 744–9
4 Hilton JF, Blaschko SD, Whitson JM, Cowan JE, Carroll PR. The impact of serial prostate biopsies on sexual function in men on active surveillance for prostate cancer. J Urol 2012; 188: 1252–8
5 Chrisofos M, Papatsoris AG, Dellis A, Varkarakis IM, Skolarikos A, Deliveliotis C. Can prostate biopsies affect erectile function? Andrologia 2006; 38: 79–83
6 Helfand BT, Glaser AP, Rimar K et al. Prostate cancer diagnosis is associated with an increased risk of erectile dysfunction after prostate biopsy. BJU Int 2013; 111: 38–43
Video: A prospective study of erectile function after transrectal ultrasonography-guided prostate biopsy
A prospective study of erectile function after transrectal ultrasonography-guided prostate biopsy
Murray KS1, Bailey J2, Zuk K3, Lopez-Corona E4, Thrasher JB1,4.
Department of Urology, University of Kansas Medical Center, Kansas City, KS, USA.
Kansas City University of Medicine and Biosciences, Kansas City, KS, USA.
University of Kansas School of Medicine, Kansas City, KS, USA.
Kansas City Veterans Administration Medical Center, Kansas City, KS, USA.
OBJECTIVE
To prospectively evaluate the effect of transrectal ultrasonography (TRUS)-guided prostate biopsy on erectile and voiding function at multiple time-points after biopsy.
PATIENTS AND METHODS
All men who underwent TRUS-guided prostate biopsy completed a five-item version of the International Index of Erectile Function (IIEF-5) and the International Prostate Symptom Score (IPSS) before and at 1, 4 and 12 weeks after TRUS-guided biopsy. Statistical analyses used were a general descriptive analysis, continuous variables using a t-test and categorical data using chi-square analysis. A paired t-test was used to compare each patient’s baseline score to their own follow-up survey scores.
RESULTS
In all, 220 patients were enrolled with a mean age of 64.1 years and PSA level of 6.7 ng/dL. At initial presentation, 38.6% reported no erectile dysfunction (ED), 22.3% mild ED, 15.5% mild-to-moderate ED, 10% moderate ED, and 13.6% severe ED. On paired t-test there was a statistically significant reduction in IIEF-5 score at 1 week after biopsy compared with before biopsy (18.2 vs 15.5; P < 0.001). This remained significantly reduced at 4 (18.4 vs 17.3; P = 0.008) and 12 weeks (18.4 vs 16.9, P = 0.004) after biopsy.
CONCLUSIONS
The effects of TRUS-guided prostate biopsy on erectile function have probably been underestimated. It is important to be aware of these transient effects so patients can be appropriately counselled. The exact cause of this effect is yet to be determined.