Video: Cryoablation after failed primary radiotherapy: study finds encouraging results
Salvage focal and salvage total cryoablation for locally recurrent prostate cancer after primary radiation therapy
Andre Luis de Castro Abreu*, Duke Bahn*†, Scott Leslie*, Sunao Shoji*, Paul Silverman†, Mihir M. Desai*, Inderbir S. Gill* and Osamu Ukimura*
*USC Institute of Urology, Hillard and Roclyn Herzog Center for Prostate Cancer Focal Therapy, Keck School of Medicine, University of Southern California, Los Angeles, and †Prostate Institute of America, Community Memorial Hospital, Ventura, CA, USA
OBJECTIVES
• To present the oncological and functional outcomes of salvage focal (SFC) and salvage total (STC) cryoablation for recurrent prostate cancer (PCa) after failed primary radiotherapy.
PATIENTS AND METHODS
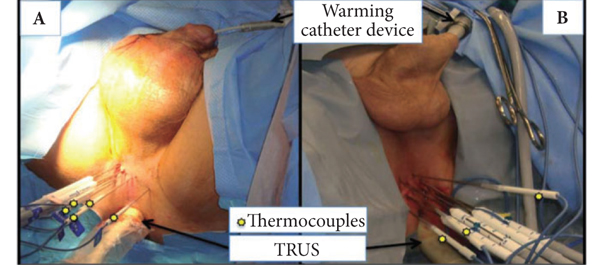
• From March 2003 to August 2010, 50 men with biopsy-proven unilateral (n = 25) or bilateral (n = 25) radio-recurrent PCa underwent SFC or STC, respectively.
• Patients were assessed after treatment by prostate-specific antigen (PSA) testing, transrectal ultrasonography, biopsy and questionnaires. Biochemical failure (BF) was defined using the Phoenix criteria (PSA nadir + 2 mg/mL).
• Data were prospectively collected and retrospectively analysed.
RESULTS
• The median pre-cryoablation PSA level and Gleason score were, respectively, 2.8 ng/mL and 7 for SFC, and 3.9 ng/mL and 7 for STC. The median follow-up was 31 and 53 months (P = 0.004) for SFC and STC, respectively.
• Oncological outcomes were as follows: no patient died; one patient who underwent STC developed bone metastases; eight patients who underwent SFC and three who underwent STC had BF and the 5-year BF-free survival rates were 54 and 86%, respectively. In those patients without BF, the mean PSA decreased by 86% for SFC and 90% for STC within the first year and remained stable.
• Functional outcomes were as follows: new onset urinary incontinence occurred in three (13%) patients in the STC group, whereas no patient in the SFC group developed incontinence (P = 0.10); Two of seven patients in the SFC group retained postoperative potency, but none of the four potent patients in the STC group recovered potency postoperatively (P = 0.48); one (4%) patient in the STC group developed a recto-urethral fistula, but none occurred in the SFC group (P = 0.48).
CONCLUSIONS
• SFC and STC are feasible and safe with acceptable mid-term oncological outcomes. For carefully selected patients, SFC is an option that could be associated with lower treatment-related morbidity compared with STC.
• Although longer follow-up and more patient numbers are needed, our initial oncological and functional outcomes of SFC and STC are encouraging.