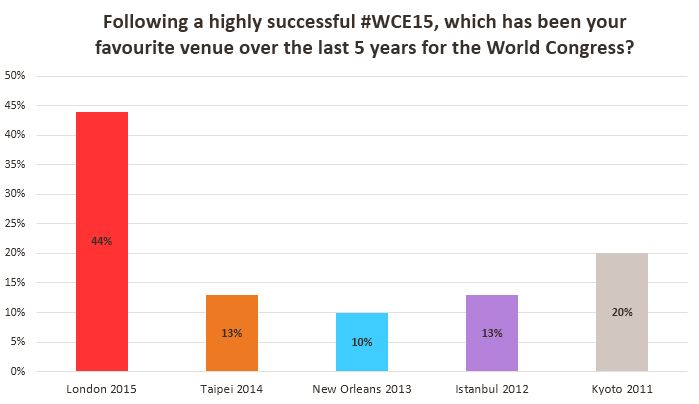
Every Month the Editor-in-Chief selects the Article of the Month from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from Dr. Ilker Gökce, discussing his paper.
If you only have time to read one article this week, it should be this one.
Significance of time interval between first and second transurethral resection on recurrence and progression rates in patients with high risk non muscle invasive bladder cancer treated with maintenance intravesical Bacillus Calmette-Guerin
Sumer Baltacı, Murat Bozlu*, Asıf Yıldırım†, Mehmet Ilker Gokce, İlker Tinay‡, Guven Aslan§, Cavit Can¶, Levent Turkeri‡,Ugur Kuyumcuoglu** and Aydın Mungan††
Department of Urology, Ankara University School of Medicine, Ankara , *Department of Urology, University of Mersin School of Medicine, Mersin,†Department of Urology, Istanbul Medeniyet University School of Medicine, ‡Department of Urology, Marmara University School of Medicine, Istanbul, §Department of Urology, Dokuz Eylul University School of Medicine Inciralti, Izmir, ¶Department of Urology, Medical Faculty, Eskisehir Osmangazi University, Eskisehir, **Department of Urology, Trakya University School of Medicine, Edirne, and ††Department of Urology, Bulent Ecevit University School of Medicine, Zonguldak, Turkey
OBJECTIVES
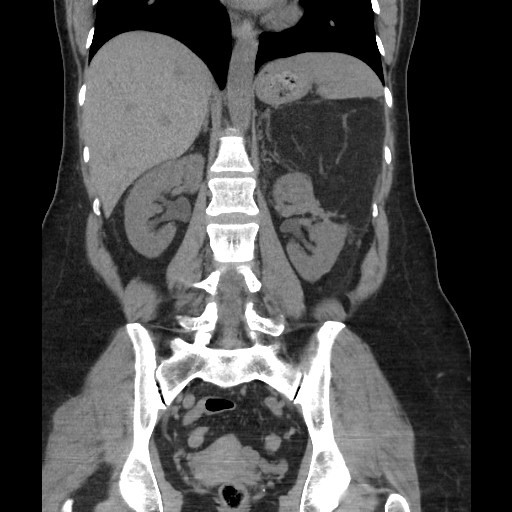
To evaluate the effect of the interval between the initial and second transurethral resection (TUR) on the outcome of patients with high-risk non-muscle-invasive bladder cancer (NMIBC) treated with maintenance intravesical Bacillus Calmette-Guérin (BCG) therapy.
PATIENTS AND METHODS
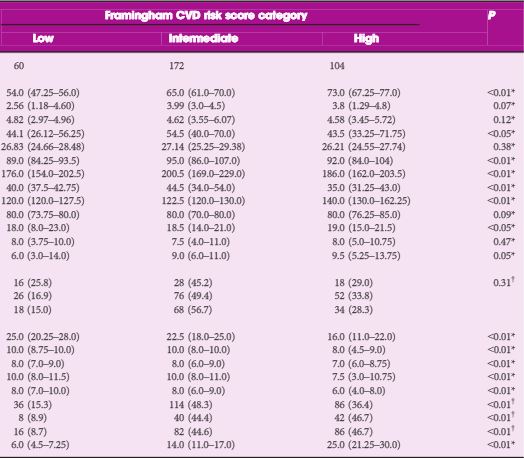
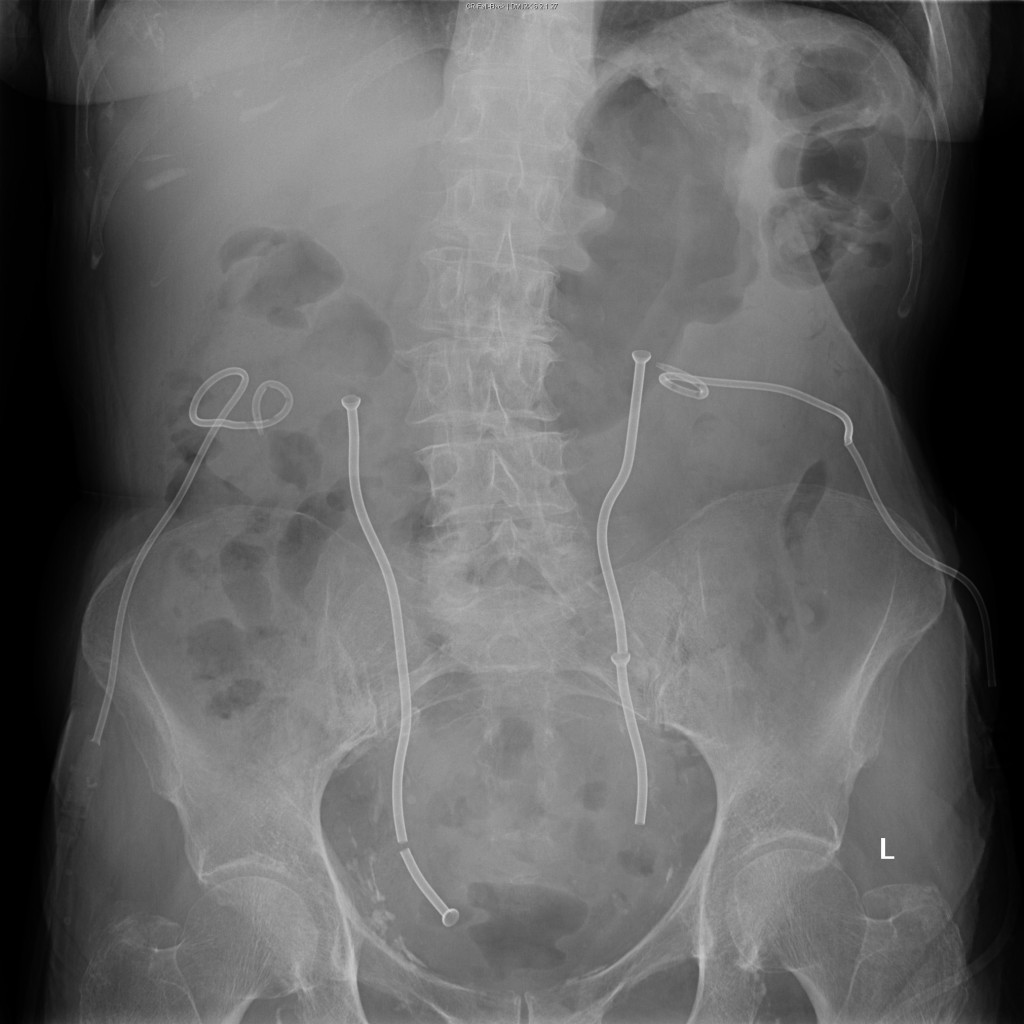
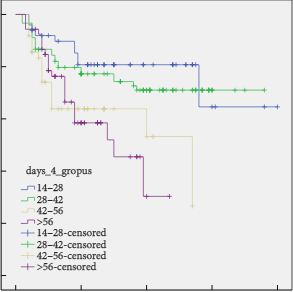
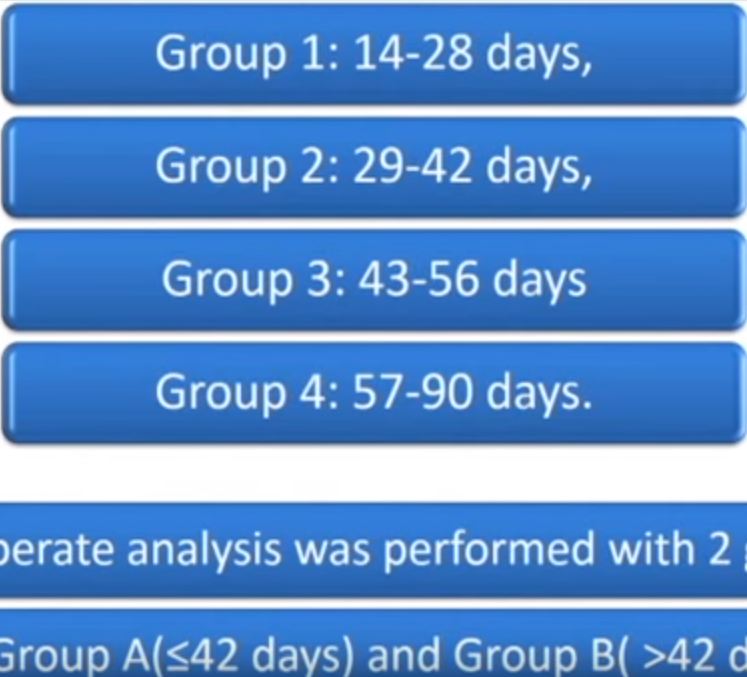
We reviewed the data of patients from 10 centres treated for high-risk NMIBC between 2005 and 2012. Patients without a diagnosis of muscle-invasive cancer on second TUR performed ≤90 days after a complete first TUR, and received at least 1 year of maintenance BCG were included in this study. The interval between first and second TUR in addition to other parameters were recorded. Multivariate logistic regression analysis was used to identify predictors of recurrence and progression.
RESULTS
In all, 242 patients were included. The mean (sd, range) follow-up was 29.4 (22.2, 12–96) months. The 3-year recurrence- and progression-free survival rates of patients who underwent second TUR between 14 and 42 days and 43–90 days were 73.6% vs 46.2% (P < 0.001) and 89.1% vs 79.1% (P = 0.006), respectively. On multivariate analysis, the interval to second TUR was found to be a predictor of both recurrence [odds ratio (OR) 3.598, 95% confidence interval (CI) 1.885–8.137; P = 0.001] and progression (OR 2.144, 95% CI 1.447–5.137; P = 0.003).
CONCLUSIONS
The interval between first and second TUR should be ≤42 days in order to attain lower recurrence and progression rates. To our knowledge, this is the first study demonstrating the effect of the interval between first and second TUR on patient outcomes.