Article of the month: Seeing the light: HAL-PDD does not lead to lower recurrence rates of bladder tumours
Every week the Editor-in-Chief selects the Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by prominent members of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
Finally, the third post under the Article of the Week heading on the homepage will consist of additional material or media. This week we feature a video from T. O’Brien and K. Thomas summarising their paper.
If you only have time to read one article this week, it should be this one.
Prospective randomized trial of hexylaminolevulinate photodynamic-assisted transurethral resection of bladder tumour (TURBT) plus single-shot intravesical mitomycin C vs conventional white-light TURBT plus mitomycin C in newly presenting non-muscle-invasive bladder cancer
Timothy O’Brien, Eleanor Ray, Kathryn Chatterton, Muhammad Shamim Khan, Ashish Chandra and Kay Thomas
Urology Centre, Guy’s and St Thomas’ NHS Foundation Trust, London, UK
OBJECTIVE
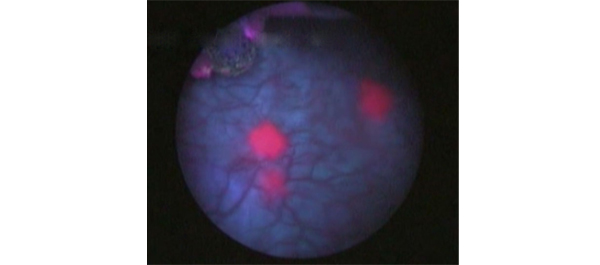
• To determine if photodynamic ‘blue-light’-assisted resection leads to lower recurrence rates in newly presenting non-muscle-invasive bladder cancer (NMIBC).
PATIENTS AND METHODS
• We conducted a prospective randomized trial of hexylaminolevulinate (HAL) photodynamic diagnosis (PDD)-assisted transurethral resection of bladder tumour (TURBT) plus single-shot intravesical mitomycin C vs standard white-light-assisted TURBT plus single-shot intravesical mitomycin C.
• A total of 249 patients with newly presenting suspected NMIBC enrolled at Guy’s Hospital between March 2005 and April 2010. Patients with a history of bladder cancer were excluded.
• The surgery was performed by specialist bladder cancer surgical teams.
• Of the eligible patients, 90% agreed to be randomized.
RESULTS
• Of the 249 patients, 209 (84%) had cancer and in 185 patients (89%) the cancer was diagnosed as NMIBC.
• There were no adverse events related to HAL in any of the patients randomized to the intravesical HAL-PDD arm.
• Single-shot intravesical mitomycin C was administered to 61/97 patients (63%) in the HAL-PDD arm compared with 68/88 patients (77%) in the white-light arm (P = 0.04)
• Intravesical HAL was an effective diagnostic tool for occult carcinoma in situ (CIS). Secondary CIS was identified in 25/97 patients (26%) in the HAL-PDD arm compared with 12/88 patients (14%) in the white-light arm (P = 0.04)
• There was no significant difference in recurrence between the two arms at 3 or 12 months: in the HAL-PDD and the white-light arms recurrence was found in 17/86 and 14/82 patients (20 vs 17%), respectively (P = 0.7) at 3 months, and in 10/63 and 15/67 patients (16 vs 22%), respectively (P = 0.4) at 12 months.
CONCLUSION
• Despite HAL-PDD offering a more accurate diagnostic assessment of a bladder tumour, in this trial we did not show that this led to lower recurrence rates of newly presenting NMIBC compared with the best current standard of care.
Read Previous Articles of the Week


After much debate as to whether this should be sent to Lancet Oncology, my friend Tim O’Brien decided that BJUI was the right home for this important and controversial paper. Thanks again.
Do not believe everything that you see??
This is a refreshingly honest piece of work which is of particular relevance to the practice of urology. Many of us have been wondering whether we should upgrade our flexible cystoscopy systems to incorporate blue light technology. Now we can hold fire on that on the basis of this important piece of evidence. Of course these data are relatively short term and a benefit may emerge with time. It will be important to keep watching this space, but in the meantime congratulations to Tim and colleagues on a useful and informative study.
This is a really important paper for all involved in bladder cancer diagnostics
Probably frustrating to those involved that there was no difference in recurrence rate seen. But I expect it is due to the Mitomycin effect and that those performing the TURBTs were excellent at it, consultant delivered cases, and learnt from having previously done many cases under blue light so that they were better white light surgeons as authors allude to. Tim, Kay and the team deserve huge congratulations for an clear and thought provoking article.
Delighted that our paper is chosen as article of the month and just as delighted to blog about it. Was I disappointed that we showed no difference in recurrence between b/l and w/l? Disappointed of course for patients that we havent unearthed the technique that leads them to the promised land of zero recurrence but as a researcher not at all disappointed. The result is the result, and is perhaps more provocative because it goes against prevailing opinion.
Optimism is a good thing in surgeons (in anyone!) but optimism about ‘new kit’ needs to be tempered. The kit may not be the key. Millions of golfers will buy expensive shiny new drivers this christmas but will their scores be lower in the new year? Probably not. Lower scores (or in bladder cancer, lower recurrence) might be more likely after a couple of lessons with the pro, some hard practice, and time on the putting green! Relentless attention to the basics is very important…