The new AUA PSA Testing Guidelines leave me scratching my head
 The fact that Otis Brawley describes the new PSA testing guidelines of the American Urological Association (AUA) as “wonderful”, should immediately raise a red flag at AUA headquarters. Dr Brawley, Chief Medical Officer of the American Cancer Society, and the most vocal anti-prostate cancer screening voice in the USA over the past decade, has enthusiastically welcomed the new document and “commended” the AUA for bringing its policy closer to that of his Society. The Guidelines have also been compared to those of the United States Preventative Services Task Force (USPSTF) which completely opposes PSA testing in any situation – a position which the AUA called “inappropriate and irresponsible” just a few months ago. Oh dear – where has it all gone wrong? ?
The fact that Otis Brawley describes the new PSA testing guidelines of the American Urological Association (AUA) as “wonderful”, should immediately raise a red flag at AUA headquarters. Dr Brawley, Chief Medical Officer of the American Cancer Society, and the most vocal anti-prostate cancer screening voice in the USA over the past decade, has enthusiastically welcomed the new document and “commended” the AUA for bringing its policy closer to that of his Society. The Guidelines have also been compared to those of the United States Preventative Services Task Force (USPSTF) which completely opposes PSA testing in any situation – a position which the AUA called “inappropriate and irresponsible” just a few months ago. Oh dear – where has it all gone wrong? ?
For those who haven’t yet seen the document, here are the five statements issued by the Guideline committee at the Annual Meeting of the AUA in San Diego this week along with some of my thoughts in italics:
- The Panel recommends against PSA screening in men under age 40 years. This appears reasonable.
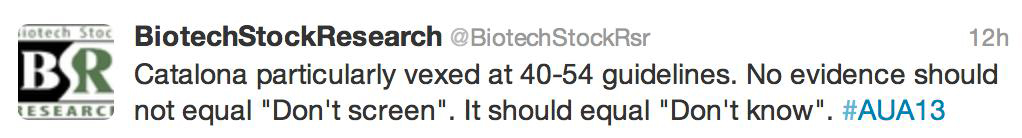
- The Panel does not recommend routine screening in men between ages 40 to 54 years at average risk. I have some problems with this (as do many others). In addition to this statement, the AUA highlights its view that the likelihood of causing harm is high and that any benefit is marginal. It appears to have completely dismissed evidence (and its own previous view), that a baseline PSA in men in this age group is highly predictive of future prostate cancer, metastasis and death. In my view, there is considerable value in having a baseline PSA in this age group and I am disappointed that the AUA has not recognised the evidence to support this.
- For men ages 55 to 69 years the Panel recognizes that the decision to undergo PSA screening involves weighing the benefits of preventing prostate cancer mortality in 1 man for every 1,000 men screened over a decade against the known potential harms associated with screening and treatment. For this reason, the Panel strongly recommends shared decision-making for men age 55 to 69 years that are considering PSA screening, and proceeding based on a man’s values and preferences. I agree with the emphasis here on shared decision-making, although the concept can be somewhat nebulous and difficult to achieve in real-life. However, I think that this statement somewhat over-emphasises the harms associated with PSA testing in this group. Rather than portray the reduction in prostate cancer mortality as being very minor (1 in 1000), men should know that when compared with a man who chooses not to have PSA testing in this age group, those who do have regular PSA testing have a 44% reduction in prostate-cancer mortality over a 14 year period. Furthermore, the numbers needed to screen (293) and number needed to treat (12) to save one life stack up very well when compared with other screening modalities such as mammography (Hugosson et al). Why has the AUA instead chosen to over-emphasise the harms? This is disappointing.
- To reduce the harms of screening, a routine screening interval of two years or more may be preferred over annual screening in those men who have participated in shared decision-making and decided on screening. As compared to annual screening, it is expected that screening intervals of two years preserve the majority of the benefits and reduce over-diagnosis and false positives. This appears reasonable.
- The Panel does not recommend routine PSA screening in men over age 70 years or any man with less than a 10 to 15 year life expectancy. Yes, but this strong advice not to offer PSA testing in men greater than 70 belies the fact that many men in this age group have a long life expectancy (eg in Australia a male who reaches 70 has a 15 year life expectancy (www.abs.gov.au), and an early diagnosis of prostate cancer may prevent their untimely death from this disease. Clearly, not all men in their 70’s are the same but following this advice to the letter could deny many men the option of avoiding death from prostate cancer in later life.
Therefore, it appears that the only circumstances under which the AUA currently recommend a PSA test be performed is for men between the age of 55 and 69 following a weekend seminar so they can be adequately informed (or thoroughly confused).
These statements have led to headlines such as these in the mass media today:
- Urology Group Stops Recommending Routine PSA Test (USA Today)
- Looser Guidelines Issued on Prostate Cancer Screening (New York Times)
- Urologists No Longer Support Routine Prostate Cancer Screening (Minn Post)
- Most men don’t need PSA test (Arizona Star)
- AUA No Longer Recommend Routine PSA Testing For Prostate Cancer (Huff Post)
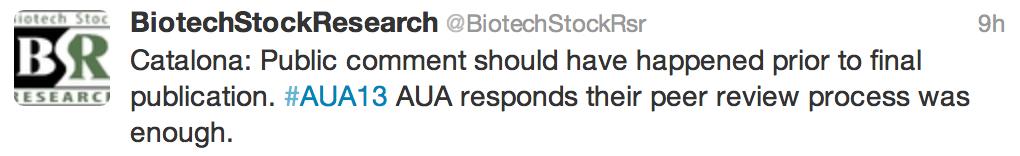
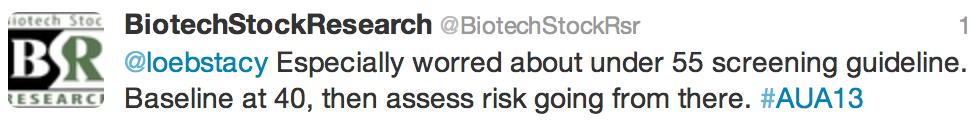
I think it is reasonable to say that this AUA document adds more confusion than clarity to the debate around prostate cancer testing. It has certainly provoked some anger among prominent members of the AUA who voiced their displeasure to the Committee during the plenary and also through social media. Dr Catalona was first to the microphone asking why AUA members were not more widely consulted prior to publication and in particular, challenging the guidance around men aged 40-54 (reported on Twitter):
Much progress has been made in the last few decades with a 30% reduction in prostate cancer-specific mortality since the introduction of PSA testing. And while we accept that this has led to a large amount of over-treatment of less aggressive disease, it is clear that (at least outside the USA), active surveillance is being enthusiastically embraced for appropriate patients. Any return towards the pre-PSA era would likely lead to a reversal in these mortality gains and we would again see many more men presenting to our rooms with incurable disease.
As Dr Smith editorialized in the Journal of Urology following the publication of the ERSPC and PLCO trials in 2009, “Treatment or non-treatment decisions can be made once a cancer is found, but not knowing about it in the first place surely burns bridges”. It is clear that many urologists consider these new AUA PSA Guidelines to be in danger of burning these bridges. However, rather than burn bridges, it is likely that urologists and others will ignore these guidelines and continue to counsel men in a more balanced fashion about the pros and cons of PSA testing. The AUA will then need to consider whether ignored guidelines are failed guidelines.
Prof Tony Costello is a Director and Professor of Urology at the Royal Melbourne Hospital, Melbourne, Australia.
Twitter: @proftcostello
Comments on this blog are now closed.





Points well made Tony. I think what has upset people is the language the AUA have chosen in the narrative around these guidelines. The emphasis appears to have shifted too far towards the negative/harm side and the balance has been lost. Also, the fact that these guidelines are meant for asymptomatic men and do not apply to those at higher risk appears to have been lost in the emphasis. The newspaper headlines you quote above seem to reflect this mixed messaging. These guidelines could have done much good but they do appear to have caused even more confusion.
Excellent, useful summary Tony. In speaking with a committee member, the voiced reason was to transition from a consensus opinion guideline to an evidence based guideline. Since the European screening study did not study the younger cohort, the panel could not include them in the study’s findings regarding men ages 55-69. I agree with you that the omission of the younger cohort from screening into the “don’t know” category surely translated into more definitive, misleading statements in the media, and the AUA had to issue subsequent clarification statements. The public commentary issue is interesting, but cannot change the evidence. So patients and physicians must continue to interpret these guidelines carefully. Further study is needed, but the Protect trial may be out in 2016 or so and may be definitive in our future strategies, i.e. the early detection model versus back to clinical/symptomatic detection.
(Sorry John didn’t see your post until mine was up)–very good points re: the focus of this guideline’s development process that underscore the limitations of the current evidence base and the need for interpretation of these guidelines as general framework, but not definitive answer to every question.
Agree with Declan and appreciate Tony’s characteristically wise perspective. To paraphrase an earlier discussion of his on this topic, we are all trying to figure out the best way of not throwing out the baby with the bathwater. The points on reduction of the morbidity of advanced / metastatic disease are mentioned in the statement but washed out in the focus on harms on the other side. On the methods side, I found it encouraging that the AUA was considering some of Ruth Etzioni’s superb CISNET modeling work in this setting–hopefully we will be able to apply more of this type of research in further considerations of practices for which randomized trials’ answers to important questions are lacking and/or problematic (among which there are many). At the end of the day, as urologists, we are still responsible for underscoring the complexity of these considerations as we engage with our patients as well as our colleagues in primary care specialties. The new guidelines–and, more, the lay press coverage of same–may muddy the water somewhat, but I would encourage everyone to carefully read through the full document to better understand its strengths and limitations when these conversations inevitably arise.
Thanks to Tony for the excellent summary!
My main concern with the guidelines relates to the age to begin screening:
1) There is level 1 evidence that screening beginning at age 50 reduces metastases and saves lives from the Goteborg population-based randomized trial. Screening in younger men with a shorter screening interval (2y vs 4y) resulted in a greater survival benefit than in the rest of the ERSPC.
2) There is also very strong evidence– albeit not from a randomized trial– to support a baseline PSA test in the 40’s. The AUA guidelines do allow for earlier screening among men who are “high risk” (on the basis of family history or race). Our group reported in 2006 that baseline PSA at a young age is actually a stronger predictor of prostate cancer than race or family history (PMID: 16442597). The use of baseline PSA for risk stratification has been validated in many populations from around the world, including the recent study by Vickers et al. showing that it predicts later metastasis and disease-specific mortality (PMID 23596126). How can we determine who is really “high risk” without a PSA prior to age 55?
I agree with the above well considered assessment of the early detection guidelines.
Although the guidelines are designed for men of average risk, and are stated not to apply to either symptomatic men or those of increased risk, they still appear overly conservative.
Recognising the desire to be evidence based, as stated by Stacy Loeb above, they fail to incorporate evidence supporting psa testing as a means of risk stratification prior to the suggested age of 55.
Further, psa testing and a cancer diagnosis is, in appropriate cases, being uncoupled from treatment. Active surveillance further protects men from morbidity.
Thanks Stacy and Matt.
This is the dilemma…we have to manage patient scenarios of all types, and yet the evidence is not uniformly available. So one approach like the EAU guidelines is to give guidance for all situations, but list which ones are attached to which level of evidence. The AUA seems to be taking the alternate approach of only giving general guidelines where the high level evidence allows it, even if that process leaves “gaps” in the guidelines.
So our challenges is to mind the gaps.
Tony
Great blog
The Malmo data would seem to strongly support risk stratification for men in their 40s; and that is the most contentious bit.
The problem in the USA has been that for 20 years almost anyone with low volume Gleason 3+3 had their prostates surgically removed and active surveillance doesn’t make you much money. This has led to this backlash against PSA as side effects of radical treatment were often greater than potential gain.
I feel it is better to know your risk and potentially your accurately graded and staged disease, and then decide on your management decision.
We need to be using active surveillance more and intervening only in men with significant disease. I will have my PSA later this year (at 40).
I have never seen a plenary session where so many people have struggled to get in to eventually completely ignore a guideline.
What a pity the AUA Guidelines neglected to incorporate the new data reported from Andrew Vickers et al.
They concluded that measurement of PSA concentration in early midlife can identify a small group of men at increased risk of prostate cancer metastasis several decades later. Careful surveillance is warranted in these men. Given existing data on the risk of death by PSA concentration at age 60, these results suggest that three lifetime PSA tests (mid to late 40s, early 50s, and 60) are probably sufficient for at least half of men.
These data are at complete variance with the recommendations from the AUA.
Once again, arguments about inducing anxiety and risk of over-diagnosis have prevailed. Why does no-one attack mammography for the same reasons? As Stacy Loeb has recently said, the issue is of over-treatment rather than over-diagnosis, and this can be overcome. As I have said, anxiety is awful, but gradual death from pelvic cancer is also pretty rough.
Terrific summary, and great comments. I’m going to go out on a limb and say that I really support what the guideline panel did. Do I agree with it whole hog? No way. Baseline PSA in the 40’s should be in there, and the flat-out recommendation not to screen men over 70 is very worrisome. But I give the panel a lot of credit for weighing the evidence in a reasonable fashion and producing guidelines that are based on a variety of high quality data sources (unlike, say, the USPSTF recs. . .). As Declan and Tony have pointed out, though, the messaging in terms of the media coverage was a complete catastrophe. We clearly could have done a better job of driving home a different message, and losing this PR battle is giving all of the PSA nihilists good cause to lick their chops.
I also support your assertions Todd, and believe that you point out one of the most critical aspects of the guidelines. To paraphrase Penson on the podium “We can only go where the evidence takes us”. The AUA guidelines reflect a synthesis of the best available high quality data sources. As more/better data mature guidelines predicated on data (as apposed to consensus opinion) should be more amenable to modification (no ones opinion is being judged). As Vickers points out in his widely cited BMJ publication “the age at which screening starts and the frequency of PSA testing is rarely justified in terms of empirical data”.
I have been brought up in a belief system supporting the early detection and treatment of prostate cancer. All evidence has been presented and interpreted through the lens of the unassailable merits of screening. The contrarian (read USPSTF) argument appears equally subject to bias, as the recommendations against prostate cancer screening predate the ERSPC and PLCO trials by many years (Screening for prostate cancer. In: U.S. Preventive Services Task Force. Guide to Clinical Preventive Services. 2d ed. Baltimore: Williams & Wilkins; 1996:119-34.)
It is only objective, high quality data that can bridge the chasms of opinion, the new guidelines appear to be progress that direction.
Agree with your points completely Tony. While ‘evidence-based’, there seems to have been less weight granted to the evidence not only that screening has been associated with a reduction in deaths from prostate cancer, but also a significant reduction in the morbidity from advanced disease – less presentation with locally advanced or metastatic disease, and therefore lower numbers of men on androgen deprivation therapy. So much is made of the “harms of treatment” when in reality I would rather undergo a curative robotic prostatectomy for early stage but significant disease with a high chance of regaining urinary and sexual function, than spend the last 5 years of my life castrate and suffering from incurable prostate cancer. Particularly as the life expectancy of men increases, one imagines there will be far greater numbers of men suffering from/with advanced disease (whether they ultimately die from it or not) if screening is abandoned. There needs to be less emphasis on whether we screen or not, and more emphasis on careful selection for treatment to ensure we still save those men with clinically significant prostate cancer yet avoid the overtreatment that has been associated with PSA testing.
What about younger men with a strong family history?
This debate is largely about risk and individual values for tolerating this risk. Clinical tools to objectify risks of screening vs. foregoing screening and to effectively communicate these risks to patients are noticeably lacking. Here’s an interesting read regarding how patient perceptions regarding the decision to screen markedly differ simply based on how the risks are framed: https://www.ncbi.nlm.nih.gov/pubmed/?term=23400279
Prokar – younger men with a strong family history fall outside the guideline, as do men with LUTS. The guideline is for men at “average risk”. But your comment helps highlight one of the main issues with these guidelines – the language and emphasis is more on harm than good and they do not adequately emphasis/explain the cohort of men who these guidelines are aimed at. This is why, despite the very evidence-based and diligent approach which the panel have undertaken, and which Todd rightly highlights, we now have more confusion than clarity.
Great blog Tony. So we mostly have some serious disagreements with aspects if the guidelines. To what degree are we oblidged to follow these if our personal interpretation of the same data is in conflict? Legally could we be held responsible for poor outcomes that stem from testing outside the guidelines? Becomes a slippery slope and we are assuming the risk in doing what most of us believe to be in the best interest of our patients. Had the guidelines left more room for clinical judgement in the younger men, we would have more latitude.
PS- For anyone who got trampled trying to enter the plenary session or who wants to hear more discussion about the new guidelines, I will be interviewing Dr. Ballentine Carter about them on the air (Sirius XM channel 81) on Wednesday May 22 at 7pm EST. Feel free to listen in, give us a call, or tweet me any questions @LoebStacy
I’m with Todd on this one. I support most of what the guideline proposes. I agree with every single point made in Tony Costello’s blog, except #2, which, to be honest, allows for some interpretation (what constitutes ‘routine’ vs. ‘baseline’ screening). In the end, a lot of Urologists are more unhappy with the media’s interpretation of the guidelines, rather than what is included.
Sometimes it’s interesting to see how and what the ‘other side’ thinks. In that regard, Otis Brawley’s book is quite interesting (https://www.amazon.com/How-We-Do-Harm-America/dp/1250015766). Read his chapters and criticism on PSA screening, the Goteborg screened population, … some interesting points there, although some may be oversimplification of a complex problem.
Terrific Stacy. Well done getting Dr Carter on your show – we will tune in from Australia. Great show by the way! I enjoyed being interviewed myself and you have had some great guests on.
We will also be tackling these guidelines at the Prostate Cancer World Congress in Melbourne in August (www.prostatecancercongress.org.au). We will have yourself, Dr Walsh, Dr Catalona, Matt Cooperberg, Martin Gleave, Vip Patel, Jay Smith, Tom Ahlering, Noel Clarke and many others here and will be generating our own consensus statement following the Congress.
Very insightful blog Tony and great to have such an in-depth review of the guidelines from one of our thought leaders. The new AUA guidelines make it obvious that it has been difficult to advocate prostate cancer screening in all men due to the conflicting evidence out there. So I have found your comments useful and I do concur with the points you have raised.
I understand some aspects of the guideline committee’s concerns regarding widespread screening. Although the ERSPC shows early screening reduced death from prostate cancer by 20% at 10yrs and metastatic burden by 31% by 12yrs, there is still a valid concern regarding the morbidity of over treating prostate cancer.
However, with the increasing validation of active surveillance for low risk disease, the physical morbidity of treatment has to be considered to be lower than touted in the arguments against prostate cancer screening. Furthermore, following on from Jim’s comment, we have little evidence regarding the anxiety experience by men undergoing active surveillance, with early data from PRIAS suggesting favourable levels of anxiety and distress in this group, rather than the reverse used in anti-screening arguments..
In addition, as Roger and Ben mentioned, the Malmo Preventive Project cohort data has shown that further prostate cancer risk stratification can be achieved by taking baseline PSA levels at set intervals in a man’s midlife. Thus we should not rule out baseline PSA when the evidence for its use shows such promise. In fact, it may make the screening process far more streamlined. This stratification may be taken to the next level with the prostate health index, which was so well presented by Stacy at this month’s AUA.
I will wait in hope, that by the next run of AUA guidelines these latter aspects will be taken into account and that the negative spin outlined by Tony and Declan, which the press have taken from these guidelines will be reversed.
In the meantime, these are guidelines and thus should guide rather than dictate our future practice.
The main issue I have with the guidelines is in the younger age groups. The AUA has gone to some lengths to state that screening = testing, and there is nothing to distinguish between the two, which I disagree with. Is there data to support mass screening in the younger age groups, probably not, but based on previous peer reviewed articles, and the recent data by Vickers et al., there is evidence that whilst the risk of dying from prostate cancer remains low, that approximately half the cancer deaths occur in the top 10% of PSA levels and testing thse men periodically may provide significant benefit. Surely it is better to risk stratify men to determine the frequency of testing, and save potentially many men rather than ignore the data and have alot of increased mortality in these younger age groups.
Having been to my GP today and informing him I’d just landed back from the American Urology ASM his eyes lit up and he eagerly probed me for the latest screening guidelines, much to his disappointment. I started to reel off the Guideline Statements but only got as far as number 2:
“But what about all the men who come to me in their 40’s asking for a PSA test? You try explaining to them why they can’t have one!”.
The confusion amongst the Urological community translates to much greater ambiguity on the front line. I certainly feel for the GPs trying to decipher all of this. I have forwarded him the new AUA guidelines and Professor Costello’s balanced perspective.
Thank you.
Ben Challacombe – Actually a viable and responsible AS plan does cost a lost of money. Repeated biopsies, color doppler tests, blood tests and quarterly consultations with docs like Dr. Scholz aren’t cheap. Try adding up those expenses over 5-7 years and see what you get.
The new guidelines are atrocious. I wouldn’t have caught my G7 at 40 and been afforded the choice of treatment with the new guidelines, I would have found out 15 years later.
Great blog Tony, all well made points. As Declan, Dan, Roger, Mark and many others have pointed out, one of the main failings of these guidelines are the screening recommendations for younger patients. How are young men and their GPs to interpret these guidelines? In response to criticisms, the AUA has emphasised that these are guidelines only and are not to be rigidly followed, but this nuance will be lost on busy frontline practitioners, just as it has been lost on the lay press. This is a step backwards and disappointing.