Article of the Week: Antibiotic prophylaxis in ureteroscopic lithotripsy
Every Week, the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Antibiotic prophylaxis in ureteroscopic lithotripsy: a systematic review and meta‐analysis of comparative studies
Abstract
Objective
To explore the efficacy of antibiotic prophylaxis and the different strategies used to prevent infection in ureteroscopic lithotripsy (URL) by conducting a systematic review and meta‐analysis.
Materials and Methods
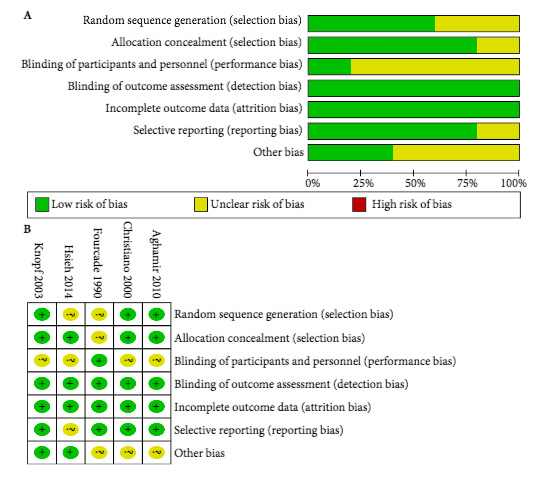
A systematic literature search using Pubmed, Embase, Medline, the Cochrane Library, and the Chinese CBM, CNKI and VIP databases was performed to find comparative studies on the efficacy of different antibiotic prophylaxis strategies in URL for preventing postoperative infections. The last search was conducted on 25 June 2017. Summarized unadjusted odds ratios (ORs) with 95% confidence intervals (CIs) were calculated to assess the efficacy of different antibiotic prophylaxis strategies.
Results
A total of 11 studies in 4 591 patients were included in this systematic review and meta‐analysis. No significant difference was found in the risk of postoperative febrile urinary tract infections (fUTIs) between groups with and without antibiotic prophylaxis (OR: 0.82, 95% CI 0.40–1.67; P = 0.59). Patients receiving a single dose of preoperative antibiotics had a significantly lower risk of pyuria (OR: 0.42, 95% CI 0.25–0.69; P = 0.0007) and bacteriuria (OR: 0.25, 95% CI 0.11–0.58; P = 0.001) than those who did not. Intravenous antibiotic prophylaxis was not superior to single‐dose oral antibiotic prophylaxis in reducing fUTI (OR: 1.00, 95% CI 0.26–3.88; P = 1.00).
Conclusions
We concluded that preoperative antibiotic prophylaxis did not lower the risk of postoperative fUTI, but a single dose could reduce the incidence of pyuria or bacteriuria. A single oral dose of preventive antibiotics is preferred because of its cost‐effectiveness. The efficacy of different types of antibiotics and other strategies could not be assessed in our meta‐analysis. Randomized controlled trials with a larger sample size and more rigorous study design are needed to validate these conclusions.