Article of the Week: Risk Factors and Timing of VTE after RC
Every Week the Editor-in-Chief selects an Article of the Week from the current issue of BJUI. The abstract is reproduced below and you can click on the button to read the full article, which is freely available to all readers for at least 30 days from the time of this post.
In addition to the article itself, there is an accompanying editorial written by a prominent member of the urological community. This blog is intended to provoke comment and discussion and we invite you to use the comment tools at the bottom of each post to join the conversation.
If you only have time to read one article this week, it should be this one.
Risk factors and timing of venous thromboembolism after radical cystectomy in routine clinical practice: a population-based study
Objective
To describe the risk factors and timing of perioperative venous thromboembolism (VTE) and its association with survival for patients undergoing radical cystectomy (RC) in routine clinical practice.
Patients and Methods
The population-based Ontario Cancer Registry was linked to electronic records of treatment to identify all patients who underwent RC between 1994 and 2008; VTE events were identified from hospital diagnostic codes. Multivariate logistic regression analysis was used to determine the factors associated with perioperative VTE. A Cox proportional hazards regression model explored the associations between VTE and survival.
Results
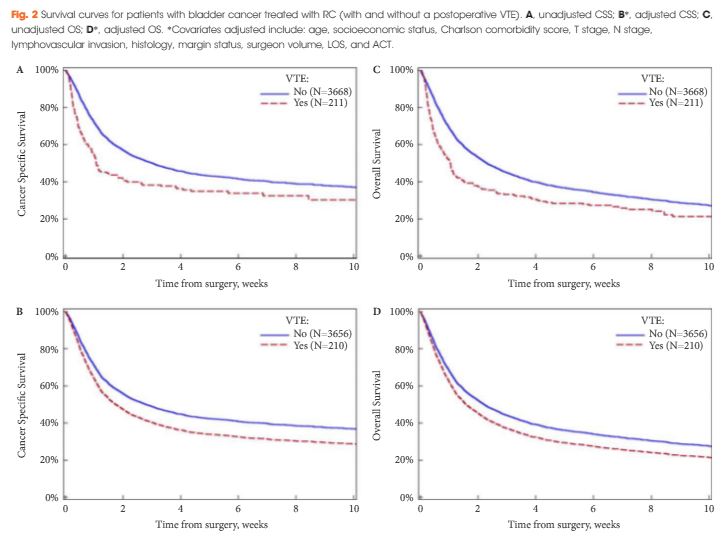
Of the 3 879 patients included in the study, 3.6% (141 patients) were diagnosed with VTE at ≤1 month of their surgical admission date. This increased to 4.7% (181) at ≤2 months and 5.4% (211) at ≤3 months. In all, 55% of VTE events presented after hospital discharge. In multivariate analysis, factors associated with VTE included higher surgeon volume (P = 0.004) and increased length of hospital stay (LOS; P< 0.001). Lymph node yield and adjuvant chemotherapy were not associated with VTE. VTE was associated with an inferior cancer-specific survival [hazard ratio (HR) 1.35, 95% confidence interval (CI) 1.13–1.62] and overall survival (HR 1.27, 95% CI 1.08–1.49).
Conclusions
Over half of VTE events in RC patients occur after hospital discharge, with a substantial incidence up to 3 months after surgery. Limited actionable risk factors for VTE were identified other than LOS. In this population-based cohort, VTE was associated with inferior long-term survival.