Editorial: Some like it safe
Since the implementation of ureteroscopy (URS) about 100 years ago, technological as well as peri-operative management improvements have made URS the treatment of choice for ureteric and renal stones. Depending on stone location and size, stone-free rates of up to 100% have been reported in combination with low peri-operative complications and short hospital stay. Endoscopic therapy of stone disease, e.g. (primary) URS, reflects the zeitgeist: minimally invasive, fast, efficient and economic. There is, however, still a lack of consensus on the question of preoperative stenting in stone management strategies. The underlying aim of preoperative stenting is to cause passive dilation of the ureter, allowing easier access to the upper urinary tract during a secondary URS.
In the current issue of the BJUI, Assimos et al. [1] report higher stone-free rates, as well as fewer complications, with the use of a JJ stent before URS in patients with renal stones, and their article, therefore, supports the previously reported findings of retrospective series with observational, multicentre evidence [2]. Their findings do not, however, corroborate improved outcomes for prestented patients with ureteric stones [1]. Notably, more stents overall were placed in the presence of renal stones compared with ureteric stones (36.4 vs 11.9%). Primary URS may not always be feasible because of anatomical abnormalities, a narrow ureteric lumen, complex ureteric path or previous instrumentation [3]. In such cases, further manipulation risking trauma and potentially long-term stricture formation should be avoided and ureteric stent placement is necessary before further therapy. Indeed, it is possible that renal stone treatment may be associated with increased ureteric manipulation; therefore, passive ureteric dilation might be helpful and facilitate endocopic access to the renal pelvis. A direct elective prestenting in these patients followed by a secondary URS, therefore, warrants discussion. Although prestenting is an additional procedure, it has the potential to lower healthcare costs by decreasing complications rates, operating time and re-operation rates, especially for large proximal stones [4].
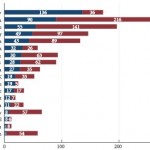
Routine preoperative stenting is not necessarily recommended by current guidelines [5]; however, the management of pre-URS stent placement is left to institutional and international practice patterns. Indeed, as shown in Figs 1 and 2 of the present paper [1], the incidence of preoperative JJ stenting varied tremendously by country. Whereas the large majority of patients with ureteric (88.1%) as well as renal (63.6%) stones were treated without a stent, in Germany, for example, >50% of patients were stented before URS. Also in China, Chile, Egypt and Israel, a higher percentage of patients with ureteric stones primarily received a JJ stent.
The use of stents is known to cause discomfort, pain and urinary symptoms, and therefore can represent significant health problems for the patient. These negatively affect daily activities, work capacity and quality of life [6]. Other disadvantages of a stenting may be higher costs associated with the need for interval procedure(s) and additional hospital stay(s). In addition, as recently reported, preoperative ureteric stent placement was not an independent predictor of stone-free status after flexible URS for renal stone removal [7].
Although there is no consensus or definite recommendation for pre-URS stenting, it should be considered and discussed with the patient when obtaining preoperative consent, especially for purely elective, non-urgent cases and in the presence of renal stones.
Long-term outcomes will show whether or not pre-URS stenting makes a difference with regard to the formation of ureteric strictures. Finally, surgical strategies need to weigh carefully the benefits to the patients and improved outcomes against cost-effectiveness.