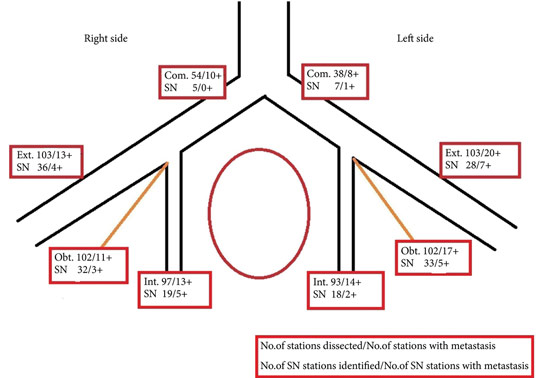
I encourage you to read the study by Aljabery et al. [1] in this edition of BJUI. Their findings are based on some very solid methodology and I think provide a robust answer to their question, which often in science means a ‘negative’ result. The principle of sentinel lymph node biopsy (SLNB) needs no introduction. It is primarily intended to detect the principal LN draining a tumour, allowing its removal and pathological determination of LN metastasis status in that individual [2].The avoidance of an unnecessary LN dissection (LND) and its associated risks is at the heart of any SLNB strategy. On the other hand, particularly for bladder cancer, there is a recognition that a higher number of LNs removed at the time of surgery confers a survival advantage to patients through more accurate staging [3]. With greater numbers of LNs removed pN0 patients are more likely to be truly N0 and pN1 patients with limited metastases have a greater chance that all disease has been completely excised. Thus, when considering SLNB in bladder cancer there is the usual conflict between maximising oncological benefit and minimising surgical harm.Aljabery et al. [1] present an excellent series of cystectomies with a 100% negative margin rate and mean LN count of 30. The 40% rate of LN involvement, is perhaps partly due to the meticulous triple sectioning of each excised LN. Their SLN technique involved four cystoscopic injections to the bladder wall surrounding the tumour and focused on the biggest lesion in multiple tumour cases. The LNs were removed in their packets and studied after removal from the patient. While this is likely to be a more precise method for determining the site of the SLN, it clearly differs from the approach one would take if trying to avoid LND in negative-SLN cases. Furthermore, examination of LNs was performed after formalin fixation. Typically when using SLN techniques frozen sections are also used to guide surgeons during surgery.The results clearly show that SLNB using radiolabelled nanocolloid does not allow accurate identification of pathologically LN-negative patients who could then avoid a complete LN dissection. Sensitivity of the technique in the detection of positive LNs ranged from 67% to 90% at the various LN stations. Overall, of patients with an identifiable SLN that was negative, 19% of patients had positive LNs elsewhere (81% negative predictive value). Effectively one in five patients who might be reassured by a negative SLN result would in fact have undetected positive LNs left behind if this technique were employed. Furthermore, this estimation does not consider errors likely to be introduced with in situ SLN identification and the use of frozen-section analysis rather than non-time-critical analysis of formalin-fixed sections.In such a dangerous disease such inaccuracy is not tolerable and so I totally agree with the authors’ [1] findings that SLNB of pelvic LNs at the time of radical cystectomy for bladder cancer is not a reliable technique for identifying LN metastasis.The positive messages from this study [1] are worth noting by those learning and undertaking cystectomy. The authors’ meticulous approach to surgery is evident from the methodology described and the accumulation of such a well-characterised series. This must be a contributing factor in achieving a 100% negative surgical margin rate and such consistently high LN yields. This should certainly be the aim of all cystectomists. The appropriate time, skill and patience should be given to this step and it should not be compromised upon, particularly when developing robot-assisted or laparoscopic cystectomy services.The findings that T-stage, N-stage and lymphovascular invasion are linked to survival are not that surprising. However, the use of LN metastatic density as a prognostic marker is interesting, as it is not usually discussed in our multidisciplinary meetings. This measure incorporates nodal tumour burden and the extent of LND. The finding of better outcomes in those with a LN metastatic density of <8% reinforces the message that even in those with LN metastases, removing greater numbers of LNs may improve prognosis. Furthermore, the finding that 30% of unilateral LN-positive tumours also had contralateral LNs settles any arguments for unilateral LN dissections.In a recent systematic review of SLNB in bladder cancer [4], the negative predictive value was found to be 92% compared to 81% in the Aljabery et al. [1] study. The authors of the systematic review suggested that SLNB is a promising technique; perhaps in view of technology advances they reviewed that might improve future outcomes of SLNB. While improvements may be possible, current evidence would not encourage me to consider SLNB using radiolabelled nanocolloid for fear of impairing cancer outcomes.
Congratulations to Aljabery et al. [1] on their work. I hope you find reading their paper as constructive as I did.
Tim Dudderidge
Department of Urology, University Hospital Southampton,
Southampton, Hampshire, UK
References
1 Aljabery F, Shabo I, Olson H, Gimm O, Jahnson S. Radio-guided sentinel lymph node detection and lymph node mapping in invasive urinary bladder cancer: a prospective clinical study. BJU Int 2017; 120: 329–36
2 Gould EA, Winship T, Philbin PH, Kerr HH. Observations on a “sentinel node” in cancer of the parotid. Cancer 1960; 13: 77–8
3 Koppie TM, Vickers AJ, Vora K, Dalbagni G, Bochner BH. Standardization of pelvic lymphadenectomy performed at radical cystectomy. Cancer 2006; 107: 2368–74
4 Liss M, Noguchi J, Lee H, Vera D, Kader AK. Sentinel lymph node biopsy in bladder cancer: systematic review and technology update. Indian J Urol 2015; 31: 170–5