Editorial: PSMA-RS – a promising utility
There is no doubt that, in the field of prostate cancer, few recent topics have been the subject of as much captivation and discussion as prostate-specific membrane antigen (PSMA) positron-emission tomography (PET) imaging. The body of literature on this imaging technique, the majority on the use of 68Ga-PSMA-HBED-CC as a radiotracer, is growing unceasingly [1], and includes data to support the superior accuracy of PSMA PET/CT for lymph node staging in prostate cancer [2] and in identifying patients unlikely to benefit from radiotherapy after radical prostatectomy [3].
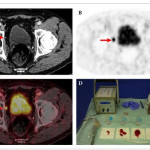
In the present paper, Rauscher et al. [4] present their data on the use of an 111In-PSMA-I&T tracer during salvage lymphadenectomy for recurrent prostate cancer. In a previous study by the same research group, 111In-PSMA-I&T has already proven to be a high-affinity radiotracer, with enhanced internalization efficiency compared with other molecules and significant accumulation in prostate cancer tissue [5].
In the present pilot study, salvage lymphadenectomy was performed in 31 patients with recurrent prostate cancer after primary treatment. Using intra-operative γ-probe measurements and comparing these with the histopathological results of the specimens, the authors found that these correlated well, resulting in a sensitivity of 92.3%, a specificity of 93.5% and an accuracy of 93.1%, with a positive predictive value of 88.9% and a negative predictive value of 95.6%.
These findings also translated well into PSA response after surgery. Postoperative PSA reductions of >50% were observed in 76.7% of patients and of >90% in 53.3% of patients. Further cancer-specific treatment was given to 33% of patients at a median of 125 days after surgery. The remaining patients remained free of treatment at a median follow-up of 337 days.
The study sample was relatively small and the analysis was conducted retrospectively. These are obvious drawbacks; nonetheless the intra- and postoperative results presented are promising. However, as the authors of the present paper point out, careful patient selection is important, and the follow-up period for these patients is still quite short. We will need to wait several years to compare the outcomes of this series with those reported in the literature with regard to salvage lymphadenectomy without prior PSMA PET CT. These data were recently published in a review by Heidenreich et al. [6]. They reported 5-year biochemical recurrence-free survival of 19–25% after salvage lymphadenectomy without the use of PSMA PET, and a median time to systemic treatment of 20–30 months [6].
As physicians, of course, our primary goal is to do the best for our patients. Certainly, we would like to believe that aggressively treating every single lesion made visible with this new imaging technique would be to the patient’s benefit. It is certainly tempting to chase these colourful lesions now demonstrated so nicely by PSMA PET/CT, but we owe it to ourselves as scientists to gather the facts and the evidence to determine whether or not our current course of action makes sense. PSMA PET radio-guided surgery is no exception to the rule, and only the evidence will tell what exact role this new technology is to have in the treatment of prostate cancer. A number of questions need to be addressed. Can we justify putting patients through surgical procedures with the morbidity associated with them? Do we not need to define oligometastatic disease in the molecular imaging era? Should we then start using PSMA PET in primary staging of prostate cancer patients? What of those tumours that do not express PSMA? Can this approach be offered laparoscopically or robotically?
It seems the introduction of PSMA PET has, instead of giving us all the answers, given rise to even more questions.
How to Cite
Geurts, N., Lamb, A. D., Lawrentschuk, N. and Murphy, D. G. (2017), Prostate-specific membrane antigen radioguided surgery: a promising utility. BJU International, 120: 5–6. doi: 10.1111/bju.13838