Editorial: TRPM8 antagonists to treat LUTS- don’t lose your cool just yet
The sensory mechanisms of the lower urinary tract enable our brain to continuously monitor the filling status of the bladder. During urine storage, low-level afferent information is mostly processed subconsciously. As the bladder fills up with urine, afferent signalling increases until we start feeling the urge to pass urine and we can consciously initiate voiding Under pathological conditions, such as urinary tract infection, overactive bladder or painful bladder syndrome, the afferent mechanisms become sensitized and lead to mechanical hypersensitivity, which is responsible for symptoms as urinary urgency, frequency and even pain.
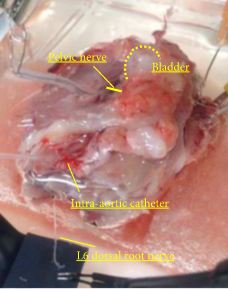
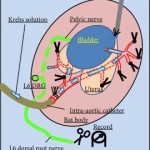
In the current issue of BJUI, Ito et al. [1] describe the role of the ion channel transient receptor potential subtype melastatin 8 (TRPM8) in mechanosensation in the bladder (detection of the bladder’s filling status). By performing continuous cystometry in freely moving rats, they show that activation of TRPM8 decreases the threshold for initiation of micturition. I.v. administration of the TRPM8 antagonist RQ-00203078 significantly increased bladder capacity and voided volume. This antagonist also prevented the facilitating effects of intravesical L-Menthol, a TRPM8 agonist on the voiding reflex. Moreover in a specialized ex vivo rat model created to study the activity of mechanosensory fibres, pharmacological blockade of TRPM8 by RQ-00203078 inhibited single-unit mechanosensitive bladder afferent activity (SAA) during bladder filling. Conversely, L-Menthol facilitated SAA in a TRPM8-dependent manner. This indicates that TRPM8 activity directly influences the sensory information that is generated by mechanosensory neurons during urine accumulation.
TRPM8 is expressed in a subpopulation of dorsal root ganglion neurons that innervate the skin and the visceral organs, including the urinary bladder. Its activity can be increased by cold temperatures (<28 °C) and cooling chemicals, such as menthol and icilin; however, TRPM8 does not respond to mechanical stimuli in heterologous expression systems, suggesting that TRPM8 affects the excitability of mechanosensory neurons rather than acts as a mechanosensor itself [2].
Two recent publications have also highlighted the importance of TRPM8 in bladder hypersensitivity disorders. Uvin et al. [3] reported the pivotal role of TRPM8 in acute cold-induced urgency. Using rats and mice, they showed that exposure of part of the skin to innocuous cold evokes bladder contractions and reflex voiding in a TRPM8-dependent manner. Their findings provide a physiological basis for the worsening of storage symptoms in response to environmental cold stimuli, as a result of activation of TRPM8. Using the oral TRPM8 antagonist PF-05105679, Winchester et al. [4] described TRPM8 as the essential cold sensor in the bladder cooling reflex in guinea pigs. Importantly, this group also conducted a phase I clinical trial using this antagonist. In their trial, PF-05105679 successfully blocked cold-induced pain in healthy volunteers who were exposed to the cold pressor test.
Altogether these data strongly support the therapeutic potential of TRPM8 modulators to treat bladder hypersensitivity disorders. Unfortunately, because of the widespread expression of these channels and their role in various homeostatic and sensory processes, pharmacological inhibition of TRP channels often leads to side effects that limit their clinical use [5]. In preclinical models, inhibition of TRPM8 leads to transient hypothermia, which was confirmed by Ito et al. [1]. They observed a dose-dependent decrease in deep body temperature after i.v. administration of RQ-00203078. In the only published clinical trial so far, PF-05105679 did not induce hypothermia but evoked a dose-dependent peri-oral burning sensation. This unexpected side effect limits the further clinical development of PF-05105679 and potentially of all TRPM8 antagonists.
In conclusion, our increasing knowledge about the functional role of TRPM8 in the urinary bladder is important to better understand the pathophysiology of functional bladder disorders, but does not yet offer an adequate therapeutic solution.