Editorial: Upper tract urothelial carcinoma: do we really need to burn down the house?
In this issue, Simhan et al. [1] use the Surveillance, Epidemiology, and End Results (SEER) database to compare outcomes of nephron-sparing and radical extirpative therapy for upper tract urothelial carcinoma (UTUC). Their study sheds some well-needed light on a difficult clinical dilemma.
A diagnosis of low- or moderate-grade, low-stage UTUC is akin to finding a spot of suspicious green mould on your attic drywall. The scale and potential danger of the problem may not be immediately apparent and both patient and urologist must make tough choices with incomplete information. Spot treat the problem and preserve nephrons via endoscopic or segmental resection or burn down the house with radical nephroureterectomy to minimise recurrence and progression risk? With only relatively small datasets for guidance and the uncertainty of endoscopic biopsy, many urologists have a low threshold to proceed with radical therapy, perhaps unnecessarily.
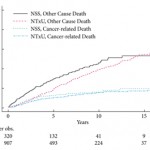
Simhan et al. [1] identified 1227 patients in the SEER dataset with low- or moderate-grade, localised, non-invasive UTUC who were treated either with nephron-sparing procedures (endoscopic resection or segmental ureterectomy) or nephroureterectomy between 1992 and 2008. For this cohort, radical therapy with nephroureterectomy imparted no advantage in cancer-specific survival. Patients undergoing nephron sparing were slightly older and did experience higher non-cancer specific mortality. This may reflect an underlying bias to offer nephron sparing to older patients with a greater burden of comorbidities and shorter life expectancy. These results corroborate another large SEER study from 2010, which documented no difference in cancer-specific mortality when comparing segmental resection with nephroureterectomy for T1–T4 N0M0 urothelial carcinoma of the ureter [2].
Population-based tumour registry studies are complementary to institutional series and are particularly valuable for rare tumours like UTUC. However, they have their limitations and these are outlined clearly in the Simhan et al. [1] article. Most notable are the lack of linked comorbidity information and the inability to separate segmental resection from endoscopic management in the nephron-sparing group. We should avoid the temptation to broaden indications for endoscopic resection to all patients with low-grade, low-stage UTUC of the renal pelvis and calyces. After all, the authors present no data on: (i) local recurrence and reoperation rates, (ii) progression to radical nephroureterectomy or (iii) correlation between endoscopic biopsy results and the ultimate pathology from nephroureterectomy specimens.
Over the past decade, there has been a progressive movement toward nephron-sparing approaches for treatment of T1 RCC, even in the context of a normal contralateral kidney. This transition has been fuelled by data showing the substantial negative impact of chronic kidney disease (CKD) on cardiovascular events and overall mortality [3]. Broader application of this philosophy to the treatment of low- or moderate-grade, low-stage UTUC would be a natural next step. This is particularly true given the advantage of maximising nephrons should disease progression necessitate platinum-based chemotherapy.
However, endoscopic resection of UTUC carries a much higher burden of local recurrence (20–85%) [4], than does partial nephrectomy for RCC. Patients with UTUC often require multiple serial endoscopic resections and years of complicated and costly surveillance. More recent data also suggests that surgically induced CKD may not carry the same risk of progression and mortality as medical CKD [5]. Perhaps burning down the house is not as potentially destructive as we once thought?
With these caveats firmly in mind, the Simhan et al. [1] study does support a growing appreciation that nephron-sparing approaches to low- or moderate-grade, low-stage UTUC do not worsen cancer-specific mortality. Although these findings are encouraging, I agree with the authors that patient selection for nephron sparing should continue to be informed by clinical judgment and adherence to published treatment guidelines [6].
Richard E. Link
Associate Professor of Urology, Director, Division of Endourology and Minimally Invasive Surgery, Scott Department of Urology, Baylor College of Medicine, Houston, TX, USA
References
-
Simhan J, Smaldone M, Egelston B et al. Nephron sparing management versus radical nephroureterectomy for low or moderate grade, low stage upper tract urothelial carcinoma. BJU Int 2014; 114: 216–220
- Jeldres C, Lughezzani G, Sun M et al. Segmental ureterectomy can safely be performed in patients with transitional cell carcinoma of the ureter. J Urol 2010; 183: 1324–1329
- Go AS, Chertow GM, Fan D, McCulloch CE, Hsu CY. Chronic kidney disease and the risks of death, cardiovascular events, and hospitalization. N Engl J Med 2004; 351: 1296–1305
- Bagley DH, Grasso M 3rd. Ureteroscopic laser treatment of upper urinary tract neoplasms. World J Urol 2010; 28: 143–149
- Lane BR, Campbell SC, Demirjian S, Fergany AF. Surgically induced chronic kidney disease may be associated with a lower risk of progression and mortality than medical chronic kidney disease. J Urol 2013; 189: 1649–1655
- Roupret M, Zigeuner R, Palou J et al. European guidelines for the diagnosis and management of upper urinary tract urothelial cell carcinomas: 2011 update. Eur Urol 2011; 59: 584–594