Editorial: Laparoscopic renal mass cryoablation: an operation in search of an indication
In this issue of BJUI, Nielsen et al. [1] report the oncological and surgical outcomes from a multi-institutional cohort of patients receiving laparoscopic cryoablation (LCA) as primary therapy for solitary renal masses <4 cm in size (cT1a). This work represents the latest addition to a growing body of literature in an important oncological space that lacks prospective/randomized evidence to guide practitioners counselling patients with kidney cancer. Although the article does not advance the discussion toward higher levels of evidence, the results are nonetheless provocative and several strengths and weaknesses deserve comment.
While nephron-sparing surgery has become the recognized standard of care for cT1a renal lesions [2, 3], the reality remains that certain patients carry unacceptable risk profiles for partial nephrectomy, making less invasive options preferable. Such indications might include being elderly or frail, having hereditary kidney cancer syndromes prone to metachronous renal tumours, or having a solitary kidney. For such patients, focal renal mass ablative techniques have emerged as a safe alternative to extirpation that avoids the permanent nephron loss associated with radical nephrectomy. From an oncological perspective, however, cryotherapy, radiofrequency ablation and microwave ablation (by any approach) all have yet to be studied against partial nephrectomy in a prospective fashion. Numerous retrospective analyses have attempted to fill the void [4], yet the general consensus among most academic kidney surgeons is that renal mass ablation offers acceptable but inferior cancer control compared with surgery [5].
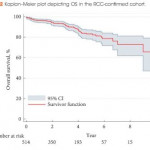
In this retrospective analysis by Nielsen et al., 808 patients underwent LCA between 2005 and 2015, 514 (63.4%) of whom had pre-procedural biopsy-proven RCC. The principal findings described in the present study include not only 5- and 10-year disease-free and overall survival, but also morbidity and mortality outcomes after LCA. The authors should be commended for the structure of their design, which included a high proportion of patients with available preoperative biopsy data. Additionally, clear definitions of treatment success, ‘residual unablated tumour’ and ‘local tumour progression’ are provided, and consistent follow-up imaging protocols were employed by the institutions involved. In each of these ways, Nielsen et al. overcome many of the pitfalls that have clouded the interpretation of results from previous reports.
Nevertheless, the oncological outcomes reported in this study, which are on a par with those for partial nephrectomy as well as other ablative techniques, must be approached with a degree of skepticism. As there is no alternative treatment cohort included in the study, omission of anatomical complexity data (in the form of nephrometry scoring) prohibits any meaningful comparison with patients having undergone ablative procedures or partial nephrectomy from other series. Availability of these data is essential for the reader to gauge the influence of selection bias in the interpretation of the results.
From a morbidity and mortality standpoint, the reported 16% overall complication rate, 3% rate of severe complications (defined as Clavien III–V) and three deaths within 30 days of the procedure might have been strengthened by the missing nephrometry data, as the rate of complications would be expected to increase with the complexity of the renal mass [6]. Also noticeably absent from the analysis are granular comorbidity and previous surgery data, both of which intuitively predispose patients to complications when undergoing minimally invasive surgery.
With these limitations in mind, the experienced kidney surgeon is not likely to see LCA as an equally effective or safer alternative to minimally invasive partial nephrectomy, which can be performed with similar complication rates and length of hospital stay without sacrificing oncological efficacy in most patients. Similarly, the question of why the practitioner should assume the risks of LCA when percutaneous cryoablation is readily available at many contemporary kidney cancer centres is unanswered by the present study. Indeed, with increasingly complex renal masses being managed via minimally invasive nephron-sparing surgery, and active surveillance of small renal masses gaining traction in the appropriate patient population, cryoablation via a laparoscopic approach unfortunately may represent another urological application without a well-defined indication going forward. We hope that the results presented by Nielsen et al. in this issue of BJUI encourage investigators to enroll patients in prospective trials aimed at comparing available ablative techniques or partial nephrectomy in matched cohorts to identify the ideal patient population for this operation and further clarify the oncological and clinical outcomes compared with surgical excision.