AUA 2014 – Friday, Saturday, Sunday: Orlando, FL
As my flight descends into the home of Walt Disney and make believe in sunny Borelando, I can’t help wonder how #AUA14 will compare to the outstanding #EAU14 meeting held just one month ago. A great meeting requires equal parts place and content, and although Stockholm is without peer, there must be a reason Orlando is the third most visited city in the U.S., right? The solution to that mystery is for another day; ask elsewhere, as I have no idea. Review of the agenda on the #AUA14 app gives hope for this meeting. There is more quality scientific content than one can possibly absorb, and highlights include the new “Crossfire” program to address controversies in urology, the John K. Lattimer Lecture by Dr. Anthony Fauci (director of the National Institute of Allergy and Infectious Diseases), the Town Hall on imaging, simulation and animation (with speakers from Hollywood who make make-believe a reality and a living), #SUO14, and the release of three new AUA Guidelines on urotrauma, medical management of stones, and cryptorchidism.
Friday afternoon kicked off with the new “Crossfire” section featuring debates on a number of heated urology controversies. Debate topics included the use of synthetic slings for stress urinary incontinence (SUI), the role of urologists in administration of therapy for advanced and metastatic prostate cancer, and the probably overly discussed topic of open versus robotic surgery (for both partial nephrectomy and radical prostatectomy). In favor of synthetic mid-urethral slings for SUI, Drs. Kennelly and Rovner presented a wealth of data showing the efficacy of slings in both the short and long term. Drs. O’Connell and Blaivas countered that the pubovaginal fascial sling provides a safer alternative, with less potentially significant complications that far outweigh the benefits of having the operation.
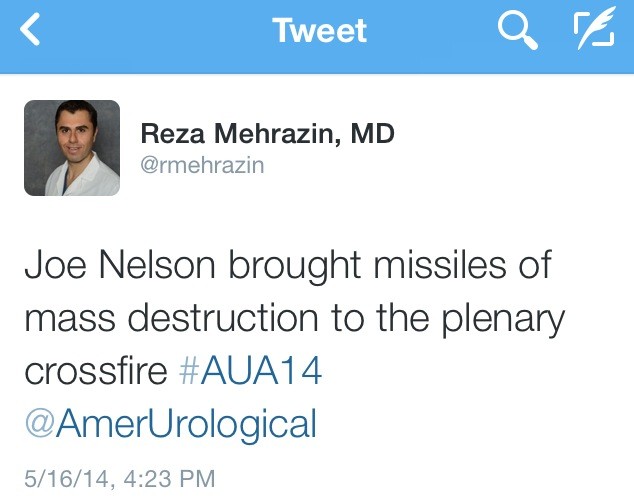
Drs. Nelson and Lepor then argued in favor of open prostatectomy, which drew some colorful tweets:
Drs. Tewari and Menon presented compelling arguments for robotic prostatectomy, and while it is hard to declare a winner, the majority of urologists in the U.S. perform robotic assisted prostatectomy; the panelists stressed that outcomes depend more upon the surgeon than the technique, and people should perform whichever approach they are most comfortable with.
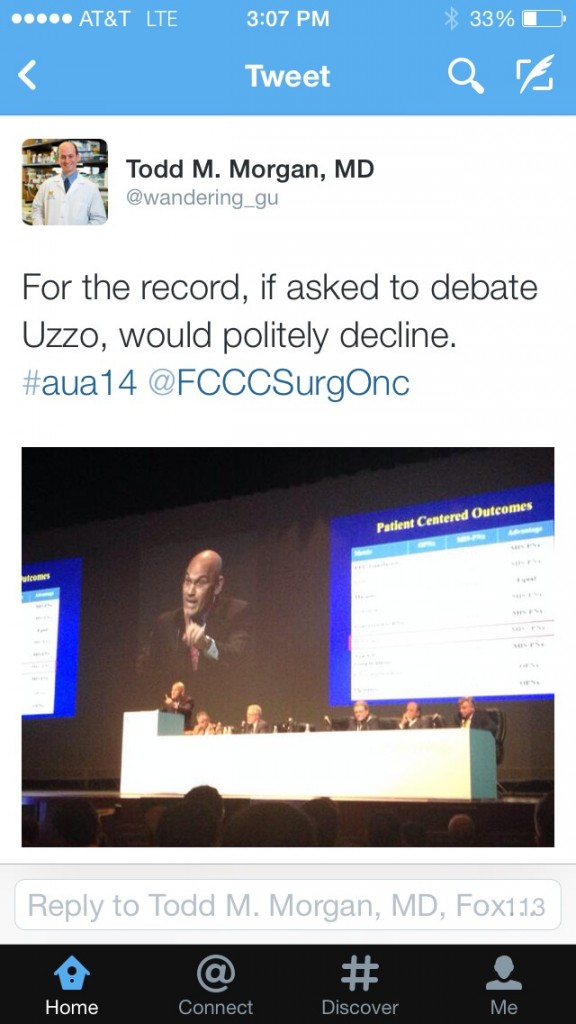
The robotic versus open debate then shifted to kidney surgery, with distinguished faculty Drs. Gill and Uzzo debating “minimally invasive partial nephrectomy is the new gold standard for renal cancer”, while Drs. Blute and Libertino argued in favor of open surgery. Although both sides had thought provoking arguments, presented data were all limited by their retrospective designs, institutional experience, or lack of validation. In my opinion, even with high volume surgeons, most patients with highly complex tumors or a renal mass in a solitary kidney undergo open surgery, which implies selection bias that limits the generalizability of robotic or laparoscopic partial nephrectomy. As contemporary experience with robotic surgery grows, we can anticipate that more complex lesions will be approached via MIS techniques in the future. We always love to throw in “randomized clinical trials are needed”… although I do think that IDEALLY prospective evidence would be great, however a clinical trial comparing MIS partial Nx to open techniques will be fraught with accrual challenges and are most likely not expected in the near future. Until more definitive prospective evidence is available, decisions regarding the optimal surgical approach for the renal mass should be determined by individual patient and surgeon preference, experience and comfort level.
Following the debate, Dr. Todd Morgan nicely summarized audience sentiment:
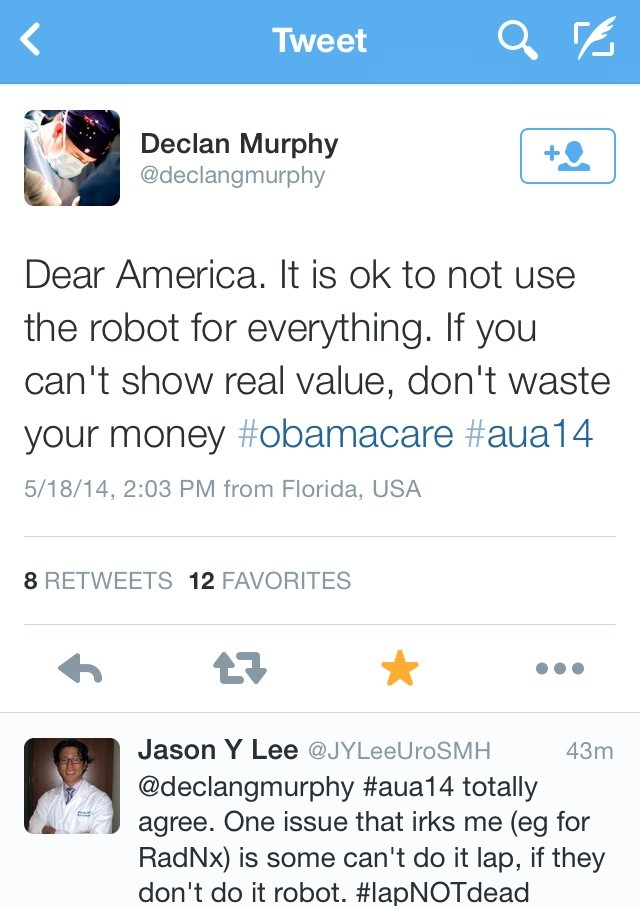
Dr. Declan Murphy provided perhaps the best sage advice regarding robotic versus open surgery:
Social Media continues to grow in urology, and Friday evening concluded with a wonderful party hosted by the AUA (@Americanurol) for the “UroTwitterati”. There was a great turnout, and #SoMe heavy hitters: @daviesbj, @declangmurphy, @dr_coop, @qdtrinh, @TheUrologist, @LoebStacy, and @Tdave attended along with “wannabe” youngsters (your current bloggers, @UROncDoc and @RMehrazin). The beauty of #SoMe is that it even allows members to participate in the meeting from home, including @uretericbud and @dytcmd. Urologists should sign up for a Twitter account and join. It is very engaging and addictive!
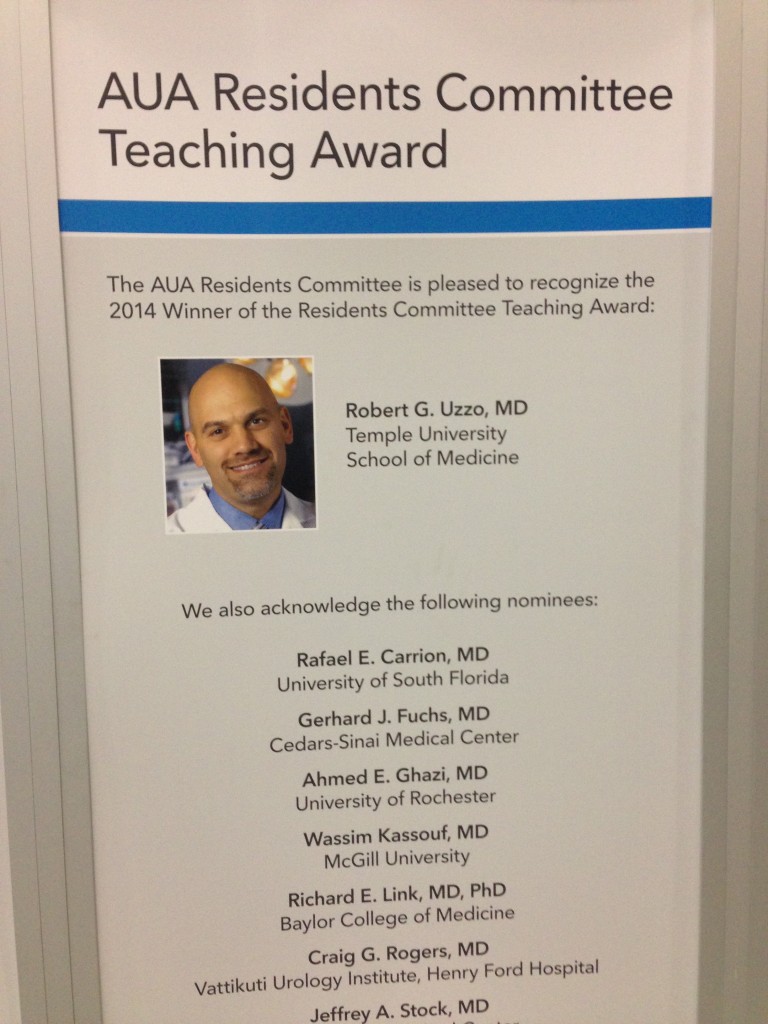
The jam-packed schedule continued on Saturday morning with the annual residents forum, during which the resident teaching award was awarded to Dr. Robert Uzzo from Fox Chase Cancer Center.
A variety of sections and societies also held meetings on Saturday. At the Association of American-Iranian Urologists, panelists Drs. Ghavamian and Samadi discussed the role of focal therapy in prostate cancer.
The remainder of Saturday was largely filled by the Society for Basic Urological Research and Society for Urological Oncology annual meetings. One highlight of the #SUO meeting was Dr. McDermott’s presentation on anti-PD-1 agents in kidney cancer. In a phase 1 RCT, Nivolumab (anti PD-L1 agent) showed efficacy for patients with metastatic RCC (n=34). There was a 29% objective response rate with a median progression-free survival time of 7.3 months. The drug was well tolerated with minimal severe adverse events, and remarkably, treatment free survival was achieved in a few patients. Immunotherapy represents an exciting and novel way target kidney cancer, and may well help usher in the era of personalized targeted therapy.
On Sunday, multiple poster and podium sessions were occurring simultaneously, which makes it hard to attend and see everything. The discussion on Twitter via #AUA14 made it possible to capture highlights from simultaneous sessions. During the Plenary session on Sunday, Dr. Fauci, Director of the National Institute of Health, Allergy and Infectious Disease Division, gave the annual Lattimer lecture. AIDS is an important topic for urologists because several aspects of the disease are specific to urology. “For example, the role of STD’s in increasing the transmissibility as well as the vulnerability of getting infected with HIV, the potential role of HPV vaccine in preventing HIV infection, and the importance of urologist issues associated with the drugs HIV patients are taking, including stones, renal insufficiency, voiding dysfunction, and erectile dysfunction,” remarked Dr. Fauci.
John P. Mulhall, Director of Male Sexual Health and Reproductive Medicine at Memorial Sloan Kettering Cancer Center, delivered the plenary state of the art lecture on radiation induced erectile dysfunction. It is an important topic, because “there are an increasing number of urologists who have hired a radiation oncologist or have a stake in an IMRT unit or do brachytherapy in their practices”, remarked Dr. Mulhall. “The pathophysiology of ED after pelvic radiation is very similar to that after radical prostatectomy based on three factors: nerve injury, arterial injury, and smooth muscle injury”.
The new AUA clinical guideline for cryptorchidism was also presented at the plenary session on Sunday. The highlights of the guideline:
- Orhiopexy is the gold standard treatment for cryptorchidism in 2014
- Initial radiographic studies are not necessary for the child with cryptorchidism
- Surgery should be performed from 6 to 18 months after birth
- Hormonal therapy should not be used as primary therapy to attempt to reposition the testis in the scrotum
Your bloggers,
Reza Mehrazin, M.D. and Jeffrey J. Tomaszewski, M.D.
Fox Chase Cancer Center, Philadephia, PA
Twitter @rmehrazin and @UROncDoc