Surgeon Responsibility
In an outstanding editorial in the current issue of the Journal of Urology (https://dx.doi.org/10.1016/j.juro.2013.05.031) my friend and colleague Jay Smith (who has accompanied us when we climbed Mt Kinabalu in Borneo and on cycle challenges in Malawi and Madagascar to raise funds for The Urology Foundation) asks the important question as to who decides when a surgeon has the requisite skills and experience to subject a patient to an operative procedure? He points out that a patient entrusting his or her quality of life, and indeed very survival, to a surgeon creates an ethical bond that has few parallels in society. Certification by the Royal College of Surgeons, American Board of Urology, or equivalent bodies elsewhere, does not imply competence in the operating theatre, or for a particular surgical procedure.
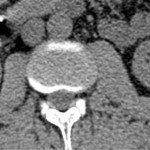
The question becomes even more pertinent in an era when new technologies such as the da Vinci surgical robot are becoming increasingly available and many clinicians, like Jay and myself, have had to become proficient robotic surgeons in the midst of their careers. Having the necessary case numbers for training, as well as expert help and mentoring in the early stages, has not always been easy. Becoming safely proficient with the robot has been compared to learning to fly a helicopter, where 40 hours mentored flying time is considered a minimum requirement.
Financial incentives, for both industry and the surgeon, and motives related to pride and practise promotion, can certainly conspire to cloud a clinician’s judgement. In the end it has to be the individual surgeon’s conscience that should be the prime determinant of whether he or she is qualified to perform any given operation. The patient trusts that the surgeon is not unduly influenced to attempt to perform a procedure beyond his or her competence. That is a truly essential covenant, as no regulatory body or oversight committee can truly know how qualified an individual surgeon may be for a particular procedure.
Patient-related outcome measurements (PROMS) and the publication of the results of individual surgeons seem set to play an important role in the future.
While some of us may view this negatively, from a patient safety viewpoint is it almost certainly the way ahead.
Roger Kirby, BJUI Associate Editor, The Prostate Centre, London




i certainly agree this is the way forward, although i remain concerns that there will be attempts to dumb down validity of outcomes if the Data and Business Intelligence in Trusts and Hospital is not up to scratch
Who better than Mahatma Gandhi can express the importance of the patient- doctor bond?
A patient is the most important person in our hospital
He is not an interruption to our work, he is the purpose of it. He is not an outsider in our hospital, he is part of it.
We are not doing a favour by serving him, he is doing favour by giving us an opportunity to do so.
-Mahatma Gandhi
Beautiful quote Krishna.
Surgeons are by nature confident people but sometimes that confidence pushes over into arrogance and poor decision making. Many disasters happen in situations that should have been avoided in the first place and no amount of technical skills can help.
They say surgeons first learn how to operate then when to operate and lastly when NOT to operate. Judgement, intuition and experience are more difficult to measure as a simulated metric but non-technical skills training is starting to look at this.
In addition to surgeon responsibility there has to be team responsibility. We have recently reported on the outcomes of the first 1000 robotic prostatectomies and the oncological outcomes from patients between 2003-5. Similarly the long term outcomes of robotic cystectomy started by our group for the first time in the EU have been published this year. Some of these patients had surgery nearly 10 years ago! The lessons I have learnt from these patients is that nearly half the problems happen outside the robotic console. As we learn to operate in teams and respect the roles played by each member, perhaps it is time to reflect on the wider responsibilities.
Herein lies the benefit of checklists. The WHO checklist reduced morbidity by 50% and mortality by nearly 30% in an international randomised trial. No robot or new drug has achieved that in recent years. Checklists reduce the “surgeon responsibility” to an extent. Almost like a fools guide. They will however never get rid of surgical incompetence which remains a matter of individual conscience as much as training and reflective, life long learning. We are planning a randomised trial of a robotics safety checklist recently published in the BJUI https://www.bjuinternational.com/?s=Checklist. All interested colleagues please contact me via this blog
I think the real question here is “Should we have a driving test for surgeons?” The Royal College of Surgeons in Ireland has looked at testing surgical competencies as a precursor for entering a surgical training programme and also as part of the tests of competency at the end of training, as I am sure most Colleges have. They have yet to implement any statutory proposals. The testing of driving a car or flying an aircraft is slightly different than operating on a live human being, but that is not to say that nothing is to be learned from driver or pilot testing. When I was sixteen we had already moved to the United States and I initially learned to drive on a Simulator, then in a car on a track and then on the road. The Simulator was also used to test some of my competencies at the end of my Drivers Education Programme. The airline industry has used Simulators for a very long time and they have been used to teach pilots how to react to emergency situations that you cannot construct in real life (i.e. a water landing of a jet plane on the Hudson). Our Editor, Prokar Dasgupta, has brought all of this simile with the airline industry to our attention and has done a lot of work on putting Simulators into our Training Syllabus and can speak to this with much more authority than I. My meagre experience in Dublin of testing basic surgical skills in a Skills Lab prior to interview for our training programme has shown a difference in level of skills of the applicants. The question is whether it will do so at the end of training. Roger’s example of the robot is the best example in surgical training. There are financial pressures and the short-cut of not taking time out to do a real training (as our Residency and Fellowship Programmes are) is not something that is easy to stand over. This blog is important and demonstrates that we cannot sit back but must look to “up our game” when it comes to training and credentialing.
Until surgical educators are unencumbered from possible litigation from trainees if said trainees are deemed not trainable, training programs will continue to graduate borderline surgeons.
When a large Asiana jet approached San Francisco airport too low and too slow recently, it resulted in the plane smashing into the perimeter sea wall with deadly consequences. It transpired that it was the pilot’s first landing at this airport in a Boeing 777 although he was an experienced pilot who had undertaken this landing in different aircraft previously. While the official inquiry is yet to determine the role of pilot error in this incident, I was interested to read this comment from Jeff Skiles, co-pilot with Chelsey “Sully” Sullenberger of the “Miracle on the Hudson” jet, in the days following the San Francisco crash: “Everybody has to have their first time,” Skiles said. “You can’t show up and have 500 hours experience in an aircraft.” And so it was for the Asiana crash pilot. However the airline industry industry are particularly good at skills training and have a world-class system of simulation and supervision to reduce the human factor in aviation incidents.
Do we have a parallel for surgical performance? Of course! We have all stepped up and done a procedure for the first time and the passenger/patient has not always been aware of this. However they trust that our respected and skilled profession has taken steps to ensure that the surgeon-in-command of the scalpel is at an appropriate level and has appropriate training and support to ensure that the patient outcome is not compromised by this being a first event.
Or consider the many surgeons who have large experience in performing open radical prostatectomy have frequently been confronted with a new aircraft type in the form of a da Vinci surgical robot arriving in their OR. I am not convinced that we do enough as a professional group to ensure that this transition is supported by adequate training and proctorship. A couple of days operating an on animal which has no prostate followed by thre proctored cases is not always enough before a solo flight should be undertaken. And unlike the passengers who have a bumpy landing due to an inexperienced pilot, the bumpy consequences of a prostatectomy can be with patients for life.
The aggressive marketing of robotic surgery has been an interesting discussion point on twitter in recent weeks. It saddens me to see marketing of such procedures beyond the training & skills of individual surgeons. I have witnessed marketing of offerings of robotic partial nephrectomy and cystectomy in spite of having never performed these procedures before. Surgeons must resist allowing the joys of new technology and the desire to expand their surgical experience/series to impact on clinical decision making and what is best for the patient. Poor or inadequate training for those in a hurry to adopt robotic surgery has been poorly addressed – professional self regulation has in my opinion been a miserable failure on this part.
Thank you for all these insightful comments Gentlemen, I appreciate them. I like Jay’s idea of an “almost sacred covenant” between surgeon and patient in his current J Urol editorial (https://dx.doi.org/10.1016/j.juro.2013.05.031). It seems to me that, increasingly, insurers in the private sector and managers in the NHS are trying to “get between” us and the patient. When surgery goes well the patient is grateful to the surgeon, when it goes badly we carry the can! We should resist the attempts of third parties to interfere with our unique surgeon/patient relationship.
There is increasing concern that current UK Trainees at the end of their training are less experienced than their previous counterparts and continue to require more education, skills and support when they take up their consultant posts in the form of mentoring. It is generally accepted that the numbers of hours required to become an “expert” is 10,000 – 30,000 and currently in the UK our trainees experience around 6,000 hours of training. Much of this is due to the impact of the European Working Time Directive (EWTD) and the government New Deal initiative on junior doctors contracts introduced in 2003. The UK conundrum shared with many other healthcare systems is how to provide effective training within the demands of service commitment and the EWTD. The concept of the learning Curve is difficult to sustain in the 21st century and should our patients really be the ones to count the cost. The challenge therefore is to devise innovative ways of training, of both technical and non-technical skills, within the limit of less hours and that training, not service, must become the priority for trainees and for those surgeons, departments and hospitals that train them. In the current climate this easier said than done.
I enjoyed reading Jay’s comment in the Journal of Urology and also these interesting opinions, particularly that of Declan Murphy, in his nicely written piece above. It must not be forgotten that the robot is not, in fact a robot, but an expensive operative tool used by surgeons. Therefore, the relationship with the patient is in no way changed. Surgery is evolving all the time and we only have to think of the huge advances in improved patient outcome in the last hundred years since, for example, Freyer reduced the mortality of prostatectomy by about 20%. It remains important, as virtually everyone has mentioned, that we maintain the high surgical standards expected of us, and that we ensure that people learning the art become expert under our close guidance.
And just in case you wanted a refresher on life long learning for surgeons, here it is… (PDF)
We are finished the day we stop learning.
The Martini clinic and MSK have incorporated robust systems of PROMS assessment to identify radical prostatectomy surgeons who are performing as outliers – at either end of the spectrum – and then have methods to assess this. I was particularly impressed by Marcus Graefens talk at BAUS – a shorter time to pad free status was noted in one surgeons results and so his surgical colleagues watched him operate, and modified their techniques to achieve similar improvement.
Requires a robust PROMS system which could be modelled on the MSK CAISIS system where patient specific feedback acts as an incentive to patients to submit their data.
Surgical outcomes can be measured objectively, and the surgeon and her conscience may not always be the best arbiter.
It is interesting that no one has so far commented on the role of mentorship in this process.
Traditional methods of training in surgery have followed the ‘see one, do one, teach one’ approach. Prior to the introduction of clinical governance, few consultants sought formal training in new procedures which were sometimes introduced uncritically. However, we have become more responsible over the years: several formal mentorship programs now exist, and I know that several mentors have given a lot of time and effort to ensure that a particular colleague is ‘safe’ at performing a given procedure, and indeed have been critical enough at times to dissuade some colleagues from taking it up.
I agree with Henry and Declan; robotic assisted surgery certainly is one of the greyest areas with regards to safety and competence; marketing and peer pressure perhaps are the main issues that contribute almost uniquely in this field. No field in urological surgery is exempt though; we need to show that we are doing more to ensure competence all around. More importantly, we need the omphaloskeptic surgeon to look instead at the mirror and decide whether he needs more training: this, I feel is going to be the biggest challenge.
I appreciate the many comments. Experience is important but a donkey can open his mouth and make a sound 1000 times and he is still not going to be singing in the opera. Surgeon skill also plays a part. A valid issue is that objective methods to judge surgeon ability are deficient but surgeons do invite regulatory scrutiny by not better policing themselves. Personal responsibility is paramount and should surely trump pride and economic incentive.
I wonder why this is limited to surgery. What about the experience or ability to manage someone’s hypertension? See a patient in the ER? What about the clarity to answer a page in the middle of the night and treat the patient appropriately? It is not just procedural experience, but rather it comes down to the very essence of placing the patient first. I wonder how much peer reporting goes on for physicians who are the bad apples. We have to help our peers identify their strengths and weaknesses, and ensure that they improve – or they will no longer be our peers. In the background of a just culture, and safety improvements, we can make a difference. We must learn from the mistakes at the Bristol Royal Infirmary and pediatric cardiac surgery.
Great discussion. Obviously a complex issue.
It is incredibly easy to assess proficiency. The placement of a single stitch at open, laparoscopic or robotic radical prostatectomy is very very telling. Operative time is a great surrogate of competency. A quick surgeon is successfully performing each movement once whilst a slow surgeon is working out what to do and perhaps attempting each step several times over. We see this when mentoring. A surgeon who has done 25% of the procedure done at 90 minutes is looking at a bad 6 hour op. that is time to get off the console and the mentor close the deal in 90 minutes expertly for the patient. Back to the simulator for the surgeon, home in a timely fashion for the mentor (!!!) and a safe outcome for the patient.
Difficult as friends tend to ask a friend to mentor them and it is a slower means of progression to bail out of a case that has been set up with a great deal if inconvenience. What would we want as a patient?
At least everyone knows now what they will get from me as a mentor!
Another reflection is my first 50 laparoscopic radical prostatectomies in 2003. A lot of slow functional recoveries and a lot of niggiliy complications. However looked after well with 100% attention to detail they do well eventually. It is more than those few hours in theatre. It’s setting up the correct case, preparing the patient and looking after them post operatively. Don’t reinvent the wheel if you have a problem. Call the mentor intra operatively or post operatively!
There are so many aspects to this discussion. Well done Prof RK.
We all want to do the best for our patients, that goes without saying. We focus on their needs and rightly so but surgical responsibility should include self reflection. As focused professional people with individual experiences who want to ‘bestow’ their expertise to the benefit of patients we should also monitor our outcomes as measured by both ourselves and our patients.
Prokar highlights the benefits and huge impact of the WHO guidelines and rightly so. When we analyse our practice the foundation and starting point of what we do should be built on what the national and international thought bodies see as current best practice.
Roger Kirby mentions the challenges of new technologies such as robotic surgery and urology as a specialism has historically forged new paths in surgery and this brings its own inherent issues and responsibilities. We need better tools to assess surgeons in training and in their day to day practice but surgical responsibility is largely about self reflection. A recent paper by Alex Mottrie highlighted the benefits of fellowship training in robotics but this is not blue sky thinking. Vickers paper on fellowship training also previously highlighted the advantages of structured training and numerous other papers have concluded large case numbers are required for complex surgery to optimise surgical technique. To state that we understand the patient comes first whilst we maintain no insight into our own limitations as technicians results in a sub optimum service to our patients.
When the Bristol enquiry assessed the failings of the paediatric cardiac surgery the reason given for poor outcomes was that the surgeons were on a learning curve. The fact that outcomes were not improving with time highlighted the poor service. On reflection this was poor surgery but what have we learned as a surgical profession? We could do worse than learn from other professions such as sports. The equivalent in surgery is mentorship. In professional sports 1 hour with a suitably experienced coach would tell who was likely to succeed as a professional sports player but more likely to identify who was not. Could someone in their 40’s expect to get signed for a professional team? Even if they showed promise their learning curve would prevent them from being an asset and yet urology an aspiring surgical speciality which readily adopts new techniques still often prioritises seniority over qualified ability.
With time I have no doubt we will develop tools to assess surgical ability and also skill development rates but in the short term we need to be honest with ourselves and prioritise patients needs above our own.
Learning curves are a difficult thing to accurately quantify but as this area of science evolves we may conclude that the optimum measures encapsulate multiple aspects.
A fast surgeon is not necessarily a good surgeon but the vast majority of good surgeons are structured in their approach and progressive. Some of the best surgeons I have seen operate, are themselves meticulous in their delivery combined with a decisiveness that makes the operation progress quickly.
An acceptable standard measure of learning curve may therefore be a combination of overall operative time with satisfactory set oncological and functional outcome rates as well as suitably low complication rates.
This should then be incorporated in an overall quantified validated score.
A really interesting discussion with some excellent points. As a non-surgical lay person, I know that I would like to benefit from the most up-to-date and effective treatment methods and be operated on by a surgeon who not only has lots of technical competence but is also sympathetic to what I might be feeling as a patient. Importantly, it would also matter to me how that surgeon was regarded by and interacted with the rest of his/her team, as team work is paramount in the OR.
The Urology Foundation exists to support and develop the best urology research, training and education that leads to the very best possible patient care. This means that we put a lot of funding into mentoring and supporting training in techniques such as robotic surgery through our robotic preceptorships, funding surgical teams and individuals to benefit from training and observing other experts, including sending teams to Guy’s and UCL and to Professor Jay Smith’s own unit in Nashville. Importantly, we also realise that just because someone may be adept at performing robotic prostatectomies does not necessarily mean that they can automatically perform a robotic cystectomy to the same competency or standard. We have therefore also sponsored skilled robotic prostatectomy surgeons to benefit from training and observing other experts in robotic cystectomies and have sponsored surgical team visits to overseas units such as Professor Peter Wiklund’s at the Karolinska Institute in Sweden.
Maybe I’ve been very fortunate in that all the urologists and surgeons I have come across have struck me as possessing very inquiring minds and a passion for furthering their knowledge and expertise. Long may that quest for knowledge and skills continue, and long may The Urology Foundation be here to try and fulfil that need!