Editorial: Fusion‐guided biopsy to guide active surveillance in African‐American men?
This timely and important article by Bloom et al. [1] highlights findings that warrant special attention in an effort to address and reduce racial disparities in low‐risk prostate cancer. At the population level, African‐American (AA) men are 76% more likely to be diagnosed with prostate cancer and 2.2‐times more likely to die from prostate cancer compared with other men in the USA. Emerging evidence suggests that racial disparities in patients diagnosed with advanced stage or higher‐risk disease may be predominantly accounted for by social factors and healthcare access [1,2]. In contrast, there is growing evidence that raises the question of whether disparities in low‐risk disease may be driven by underlying tumour and/or biopsy misclassification differences [2,3,4].
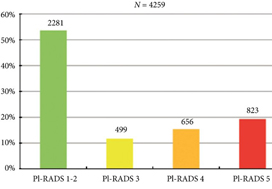
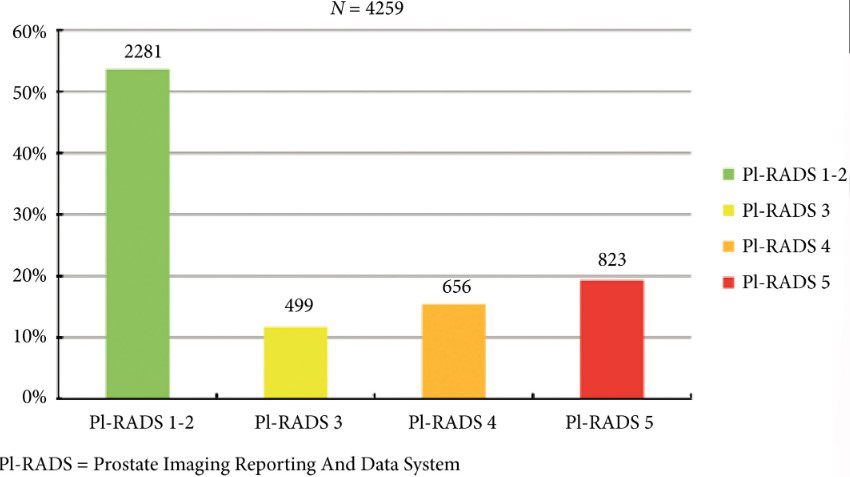
Bloom et al. [1] examined a USA study cohort from the National Cancer Institute (NCI) and found that amongst men referred to the NCI with a prior 12‐core systematic biopsy (SB), AA men with Gleason Grade (GG) 1 disease were nearly twice as likely to be upgraded by targeted multiparametric (mp)MRI fusion‐guided biopsy when compared with non‐AA men. These findings are consistent with contemporary data in the USA‐based Surveillance, Epidemiology and End Results Program, where amongst 20 125 men (including 2594 AA men) with clinical National Comprehensive Cancer Network (NCCN) low‐risk prostate cancer (GG 1 on biopsy) who underwent radical prostatectomy (RP) from 2010 to 2015, AA men were more likely to have pathological upgrading at the time of RP when compared with non‐AA men (47.3% vs 45.3%; adjusted hazard ratio 1.12, 95% CI 1.03–1.22, P = 0.007; unpublished analysis). Furthermore, the study findings are consistent with prior work that has shown that AA men with NCCN very‐low‐risk disease who underwent RP were more likely to have disease upgrading at RP (27.3% vs 14.4%; P < 0.001), positive surgical margins (9.8% vs 5.9%; P = 0.02), and higher Cancer of the Prostate Risk Assessment Post‐Surgical scoring system (CAPRA‐S) scores [5]; notably these AA men with very‐low‐risk disease also had a distinct zonal distribution of prostate cancer when compared with other men, with anterior tumours that are more difficult to sample by standard 12‐core SB alone [3].
Although low‐grade/risk disease is considered prognostically favourable and can be managed conservatively with active surveillance (AS), racial differences in outcome and zonal distribution of disease observed in favourable‐risk cohorts has led to controversy over the use of AS in AA men. Furthermore, conservative management trials have severely under‐represented patients of African descent. In this setting, most treatment guidelines advise caution when applying AS to AA patients. As such, although AS rates for low‐risk disease have nearly tripled in the USA from 14.5% to 42.1% from 2010 to 2015, there is lower relative uptake of AS for AA men compared with other men, even after adjusting for socioeconomic status, suggesting that providers and patients may be ‘risk‐stratifying’ AA patients with low‐risk disease into a higher‐risk category, and therefore less willing to proceed with AS [6].
Ultimately, the application of AS to AA patients with low‐risk disease will remain controversial and providers will make decisions based on observational data until a representative trial can help answer: (i) whether AA men diagnosed with low‐risk disease who are eligible for AS might be more likely to have distinct aggressive disease features compared with non‐AA men, and (ii) whether there might be strategies, such as guided‐fusion biopsy and/or incorporation of tumour genomics prior to AS, to help identify AA patients with underlying aggressive disease and appropriately select AA men with low‐risk disease for AS protocols.
The most interesting and important result found by Bloom et al. [1] is that amongst men who underwent mpMRI fusion‐guided biopsy after initial diagnosis of low‐risk disease on SB and who ultimately were continued on AS (those who were upgraded at the time of fusion‐guided biopsy became ineligible for AS), AA and non‐AA men had similar progression rates on AS. This result suggests that incorporation of techniques such as mpMRI and fusion biopsy may help better select AA men for AS when compared with standard 12‐core SB. Specifically, MRI guided‐biopsy may reduce disparate misclassification errors by increasing detection of higher grade and more anterior tumours that are more likely to be found in AA men who initially present with low‐risk disease after standard SB. As such, this strategy may represent one mechanism to better select AA men for AS and therefore may be able to reduce disparities in low‐risk disease.
The authors should be applauded for their important work, and this study builds on a growing body of evidence that clearly demonstrates the need for prospective trials examining different diagnostic/prognostic strategies that may reduce disparities in low‐risk disease by more appropriately selecting AA men for AS strategies.
by Brandon A. Mahal (@BrandonMahal)
References
- , , et al. Evaluation of the contribution of demographics, access to health care, treatment, and tumor characteristics to racial differences in survival of advanced prostate cancer. Prostate Cancer Prostatic Dis 2019; 22: 125– 36
- , , , Prostate cancer‐specific mortality across Gleason scores in black vs nonblack men. JAMA 2018; 320: 2479– 81
- , , , , , Pathological examination of radical prostatectomy specimens in men with very low risk disease at biopsy reveals distinct zonal distribution of cancer in black American men. J Urol 2014; 191: 60– 7
- , , Prostate cancer genomic‐risk differences between African‐American and white men across Gleason scores. Eur Urol 2019; 75: 1038– 40
- , , et al. African American men with very low‐risk prostate cancer exhibit adverse oncologic outcomes after radical prostatectomy: should active surveillance still be an option for them? J Clin Oncol 2013; 31: 2991– 7
- , , et al. Active surveillance for low‐risk prostate cancer in black patients. N Engl J Med 2019; 380: 2070– 2